What is the main difference between SOAP notes and DAP notes?
SOAP and DAP notes are both a type of progress note used by mental health professionals such as psychotherapists, counselors, psychiatrists, and clinical psychologists.
Often, we’re not taught about all the note types available to us.
This article explains the difference between the two progress note types so you can better understand the benefits of using one vs. the other and the best use cases for each.
We hope this helps!
SOAP notes vs. DAP notes
SOAP and DAP notes are two of the most widely used progress note types.
While the SOAP note is divided into four sections: the Subjective, Objective, Assessment, and Plan sections, the DAP note combines the Subjective and Objective information into one, more general, Data section. The rest is the same.
Which you choose to use is up to you as a healthcare professional and the clinical context of your client’s case. But let’s get into the two note types in more detail.
As you can tell from the acronym, one has four sections while the other only has three, and this is significant as it leads to the main difference between them.
So which note type should you use?
All progress notes serve to create a cognitive framework for clinical reasoning.
They present a structure for evaluating the client’s state and progress and serve as a communication document between different team members and other healthcare professionals (Poder et al., 2023).
Which you choose to use depends mainly on the clinical context, as well as your preferences. Read on for more about each note type, before we compare the two against each other.
More about SOAP notes
SOAP notes are a detailed and more structured note type. They emerged as medical notes and so are widely adopted in healthcare.
This can be beneficial when working as part of a larger team, such as with clients who may require a multi-person team composed of a social worker, counselor, and psychiatrist.
The standard SOAP note structure consists of these four sections:
- Subjective (S): Patient's stated experiences, feelings, and concerns.
- Objective (O): Observable and measurable data collected by the clinician.
- Assessment (A): Clinician's professional judgment and diagnosis.
- Plan (P): Treatment plan, follow-up, and next steps.
The subjective section allows for direct quotes and other self-reported client information, which can then be contrasted with the clinician’s more objective observations in the next section, giving both an unbiased view of the patient’s experience and a clinician’s full observations about the client’s account.
When the two differ, this is especially useful. For example, a clinician may observe flat affect and slower physical movements typical of depression. However, the client may report “feeling fine” despite physical evidence to the contrary, giving deeper information about the client’s emotional awareness and body connection.
You can read more about that here, and can even get a downloadable SOAP note template.
More about DAP notes
The DAP note format is a slightly streamlined version of SOAP and it is used in much the same way. As with SOAP notes, a clinician following the DAP note format will record data that corresponds to each section of the structured note, reflecting its acronym.
Since DAP notes have a section less, they’re regarded as brief and faster to write.
Unlike in a SOAP note, all clinician-observed and client-reported symptoms are combined, so you don’t have to spend time separating the subjective and objective data.
- Data (D): What happened in the session? Observations, direct quotes, objective details (appearance, mood, behavior) including elements of the MSE.
- Assessment (A): Your interpretation of the clinical data gathered, diagnoses, any progress towards treatment goals, and a re-evaluation of current interventions if needed.
- Plan (P): What you plan to do in future sessions based on your assessment of this one. Includes both the client’s next steps and your own goals as their therapist. Doesn’t need to be the entire treatment plan.
To see how you can write a DAP note based on a real-life clinical example, see here.
SOAP and DAP compared
Let’s look at the benefits of both SOAP and DAP notes side by side to help you identify when you should use which template. Although each clinician is free to decide their preferred option, it’s helpful to learn about the benefits of each beforehand.
As you can see, both are useful depending on what you’re facing together with your client, and as a healthcare provider. Yes, the DAP note can save time by combining the data you gather during a session into one – meaning you don’t have to think too long and hard about how to separate the data further.
On the other hand, this can be a disadvantage if you need to carefully monitor both the client’s and your own clinical progress over time, and need to easily track and see changes from your own and the client’s perspective.
From a legal, ethical, and insurance perspective
So far, we’ve been considering mainly the clinical perspective when evaluating progress notes. As a licensed mental health professional, it’s your duty to carefully document the interactions between your client and yourself.
This helps manage client care efficiently and allows healthcare and insurance providers to easily read and understand a client’s progress and history.
Happily, from a legal point of view, it doesn’t matter which note type you use. As long as you’re documenting sessions as is legally required and clinically appropriate for the client, the template you choose is entirely up to you.
The same goes for insurance companies, although they prefer not to have to decipher your individual shorthand (more on that here). Otherwise, you can use whatever note type suits you best.
Using a template that makes progress notes as insurance-friendly as possible and reflects the needs of the client can be both time-saving for you and treatment-enhancing for the client since insurance companies must be able to see the need for, and response to, the treatment you’re providing.
As such, choosing the right template does come with certain requirements. That said, whether you choose a SOAP or DAP note it’s unlikely you’ll go horribly wrong.
Conclusion: What is the main difference between SOAP and DAP notes?
Both note types are used by psychiatrists, therapists, psychologists, counselors, social workers, and more, to present a patient’s health findings in a clear and organized manner.
However, unlike in the SOAP note, all clinician-observed and client-reported symptoms are combined in a DAP note, making them briefer and yet more flexible when writing about the client. This can be both an advantage and a disadvantage, depending on your clinical context or situation and needs.
Unless you work in a larger practice or organization that requires you to use one or the other note format, it’s always up to you which note type you choose to use for documenting your therapy sessions.
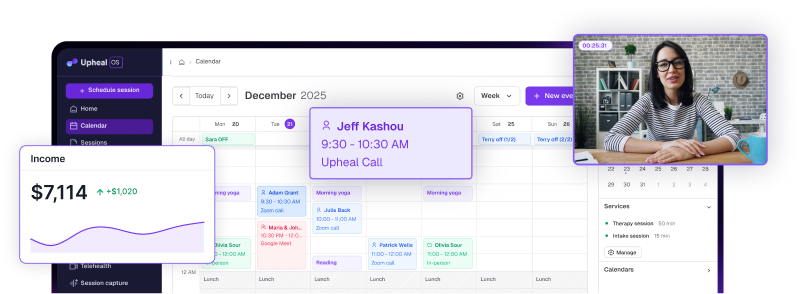
Just as we learn in therapy, you have the power of choice! That means you can always change your mind. And thanks to Upheal, you can also change to any note type easily, at any point after a session if you find it’s necessary – and without any of the manual work.