A new way to run your private-pay practice
Recent updates
See the latest product updates and improvements to Upheal.
See the latest product updates and improvements to Upheal.
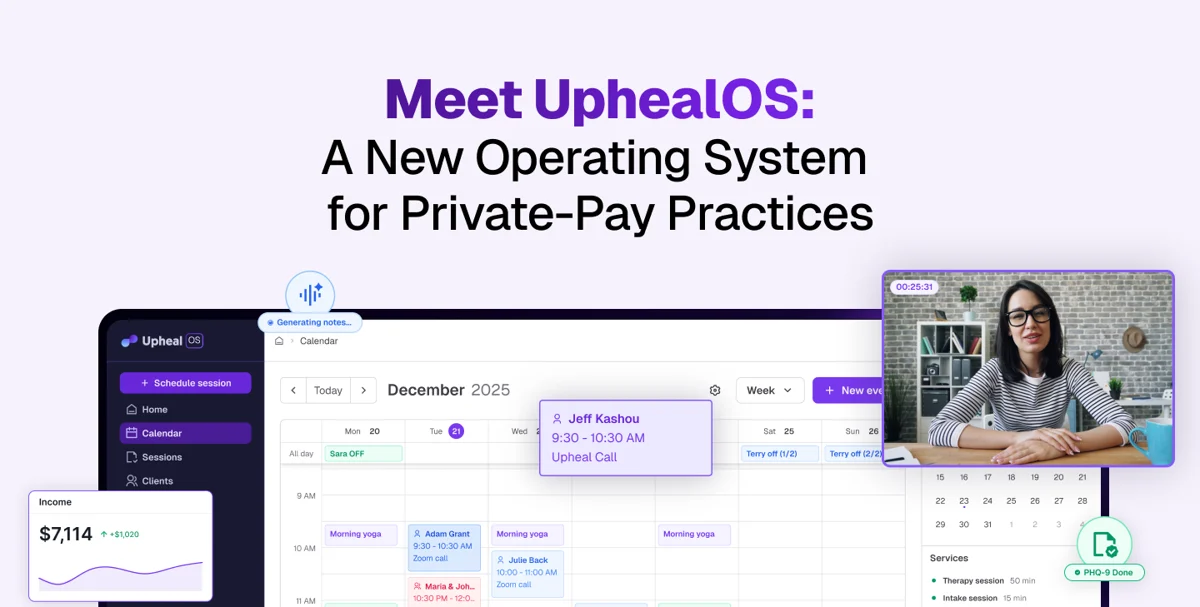
The first phase of UphealOS: an operating system for private-pay practices is here.
A new EHR-replacement that brings all the tools needed to run your practice into one AI-powered system: EHR, payments, scheduling, documentation, telehealth, practice forms, and marketing — all under a single subscription. Here's your first look at the Early Access features now available:
Get paid with ease while keeping more of what you earn. Upheal offers secure payment processing with low fees of 2.9% + $0.30, easy invoicing, and automatically generated superbills.
Collect intake and consent information quickly using customizable forms, ready-made templates, and automatic reminders that keep clients on track.
Connect and manage all of your calendars in one place, reduce no-shows with automated reminders, reschedule with ease, and offer clients a smoother booking experience.
Enjoy secure and stable virtual sessions with built-in AI. Let clients join instantly (couples and family too). Go directly from session to session by managing your virtual waiting room.
Capture sessions in real time as AI drafts structured notes for you, supports non-session documentation, and keeps everything consistent with your templates.
Reduce admin time with AI assisted treatment plans, customizable templates and automatically generate summaries.
Maintain a single source of truth for diagnostic information with synced profile, easy in-note editing, and ICD codes that flow directly into superbills.
Learn more about UphealOS here.

The simplest, most reliable way to get notes from online sessions is here: Our desktop app for MacOS, Upheal AI Notes.

Clinicians have been asking for this, and we listened.
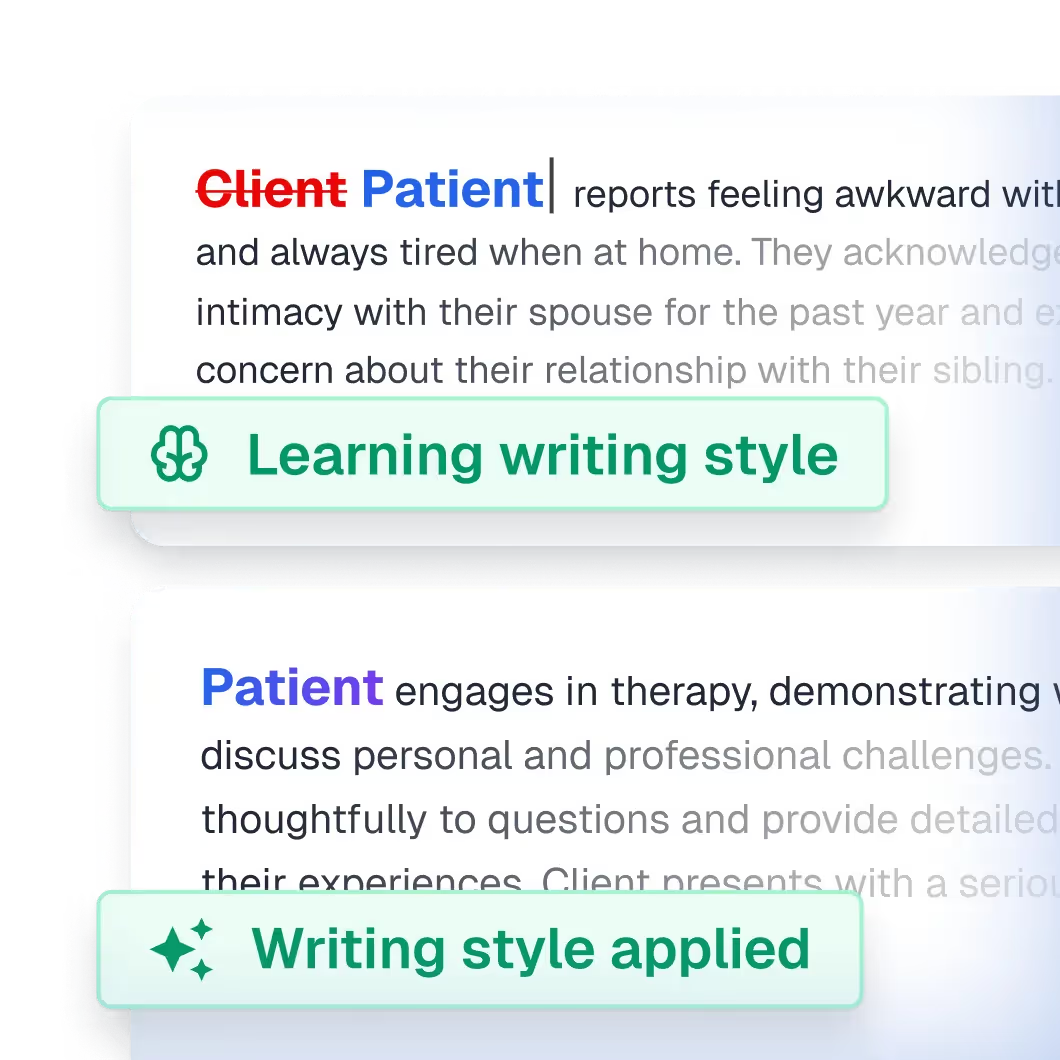
One of our most requested features is here: automatically generated notes that sound just like you wrote them.
We’re excited to launch Note Personalization. With it, Upheal AI learns your writing style, so future notes reflect your own clinical voice. The more you edit, the more AI adapts to your clinical and editorial style, reducing repetitive changes and saving you time.
Watch Jeff Kashou, LMFT, walk you through the new feature in this short video:

We're thrilled to introduce Compliance Checker: our answer to the documentation uncertainty that's plaguing private practice. It helps spot missing elements in your notes based on real payer standards, so that you can be audit-ready at all times.
This isn't another template system that forces your unique clinical voice into rigid boxes. Instead, Compliance Checker analyzes your existing documentation approach and identifies specific gaps that could trigger claim reviews. It examines treatment necessity justification, progress measurement, risk assessment completeness, and diagnostic consistency — the four pillars that determine whether your notes will survive automated review systems.
Here's our Senior Clinical Product Lead, Jeff Kashou, talking through how Compliance Checker can safeguard your practice!
Compliance Checker is currently available on Upheal's Premium plan. Try it out today with either your own or an Upheal-generated note, and have peace of mind knowing that your notes are audit-ready.
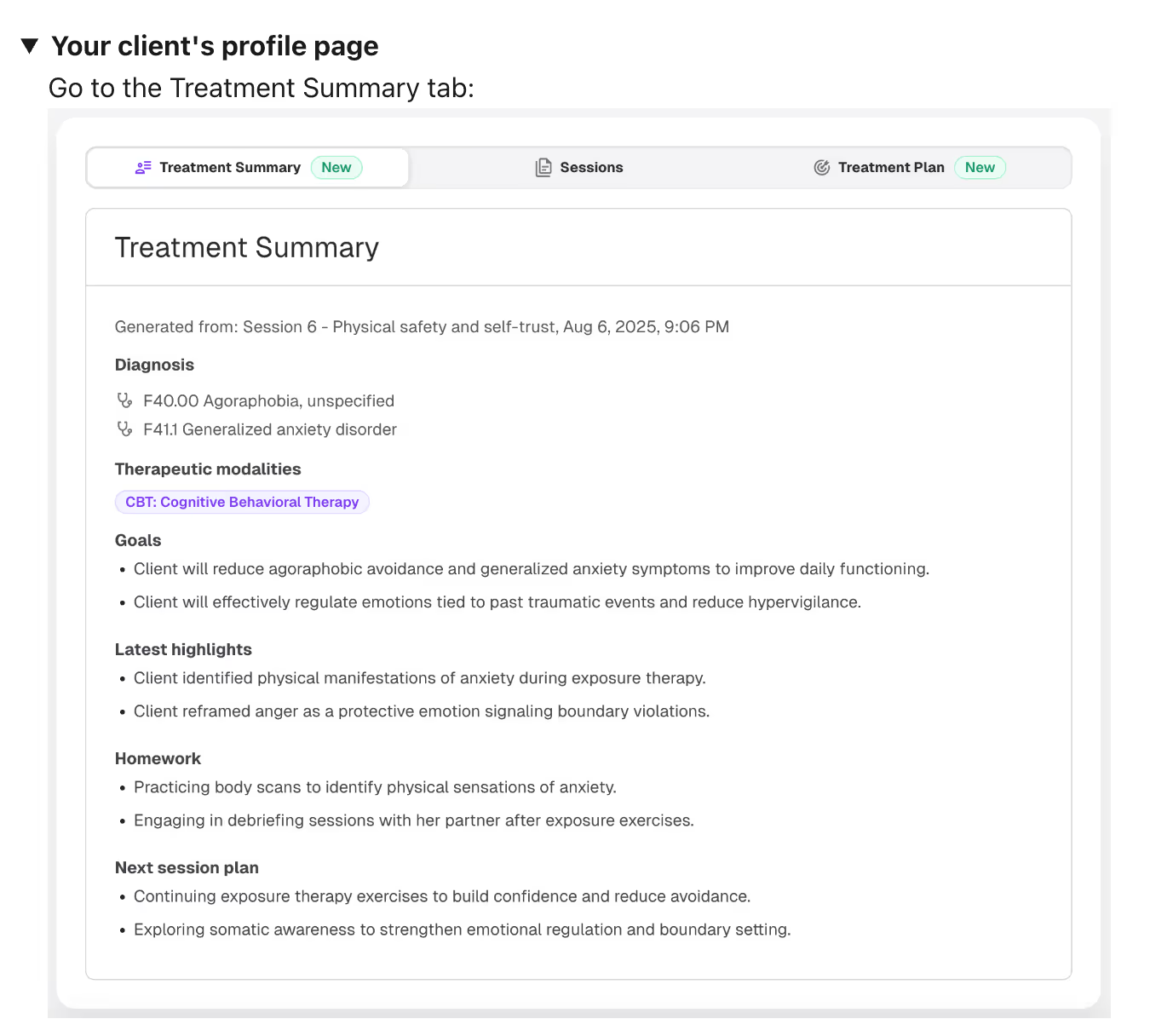
You know that anxious feeling of seeing an upcoming client session, and hastily trying to pull up notes to remember what was last discussed?
With our latest release, we hope to make that anxiety disappear!
We're excited to introduce Treatment Summaries, a new feature to help you prepare for your next session with your clients. This update is designed to save you time by pulling up important client information such as their current diagnoses, therapeutic modalities, goals from the treatment plan, last session highlights and homework assigned.
To help you stay prepared, you will automatically see a treatment summary within the Upheal calendar, in our Chrome extension, and even in our video-calling platform.
Here's a video walkthrough from our Senior Clinical Product Lead, Jeff Kashou!
This feature is currently only available on Upheal's paid plans. Try out Treatment Summaries and enter your sessions more prepared to deliver care to your clients.
.avif)
Clinical documentation should reflect the full spectrum of therapeutic interventions, not limit practitioners to generic templates. That's why we've expanded our supported modalities to 70 comprehensive approaches, ensuring your notes capture the nuanced reality of evidence-based practice.
What's new in our modalities library?
Our modalities framework now encompasses individual therapy approaches from foundational CBT and psychodynamic work to specialized trauma interventions like EMDR and Brainspotting. Couples and family systems practitioners gain access to evidence-based frameworks including Emotionally Focused Therapy, Imago, and Relational Life Therapy.
Each modality integration includes specific documentation templates that capture intervention-specific language, theoretical frameworks, and outcome measures. Whether you're documenting somatic experiencing sessions, tracking DBT skills acquisition, or noting family systems dynamics, your clinical voice remains authentic while meeting documentation standards.
The expansion reflects our commitment to supporting diverse therapeutic approaches without forcing practitioners into restrictive templates. Your clinical expertise drives the documentation process, with AI assistance that understands the theoretical foundations underlying your interventions.
All 70 modalities are available now across all plans, building on our foundation of comprehensive clinical documentation support.
.avif)
You know that frustrating routine after every session? Finish talking with your client, then spend 15-20 minutes copying notes from one system to another, fixing formatting, and making sure everything looks right. It's the kind of busy work that keeps you away from what you actually love doing.
Smart Fill fixes all of that.
Smart Fill is a Chrome extension that lives right in your browser. When you're ready to move your notes to your EHR, just hover over the Smart Fill button. You'll see purple highlights show up around the fields that will get filled—so you know exactly what's happening before you click.
Then you click once. That's it. Your complete note transfers over with all the formatting intact.
Smart Fill plays nicely with the platforms most therapists already use:
No need to learn new software or change how you work. It just makes your current setup better.
Smart Fill reads your EHR template and matches it to your Upheal notes. As long as your section names match up (like "Session Notes" in both places), it knows exactly where everything goes.
Got custom templates? No problem. Smart Fill works with those too, as long as the section names are the same in both systems.
Ready to save 20 minutes on your next note? Here's how to use Smart Fill for the first time:
💡 Troubleshooting tip: If something doesn't transfer right, it's usually because section names don't match exactly. Just rename your sections so they're identical in both systems.
That's it! Most therapists are completely comfortable with Smart Fill after using it just 2-3 times. You'll wonder how you ever lived without it.
.avif)
We're excited to introduce Golden Thread, our comprehensive AI treatment planning system that creates seamless connections between assessments, treatment plans, and progress notes. This feature addresses one of healthcare's most persistent challenges: achieving the "golden thread" standard of integrated documentation that payors demand but clinicians struggle to maintain.
Golden Thread analyzes your sessions to identify treatment priorities, suggest evidence-based interventions, and create plans that guide your ongoing work. Your progress notes now automatically connect to specific client goals, creating clear therapeutic narratives that insurance companies understand.
The system works with SOAP notes, Enhanced SOAP notes, and Upheal's native template, with support for all templates coming soon. Simply select up to three sessions to generate a comprehensive case snapshot, review and refine your AI-generated treatment plan, then watch as your ongoing notes automatically reference relevant goals.
Golden Thread is available now on Premium plans. Create your first treatment plan by opening any client profile and selecting "New Treatment Plan."
.avif)
Documentation should reflect your unique therapeutic approach, not force you into rigid templates. That's why we're introducing Smart Sections - a feature that lets you teach our AI to write notes in your clinical voice using custom prompts.
Smart Sections work by allowing you to craft detailed prompts that specify exactly what information to capture and how to present it. Whether you're tracking ERP exposures, documenting trauma processing, or monitoring couples therapy dynamics, you can create sections that align perfectly with your practice.
The key is specificity: tell the AI your preferred format, reference your theoretical approach, and include examples of your ideal output. You can even provide samples of your own writing style to ensure consistency across all notes.
Smart Sections are available now with Premium plans, building on our foundation of 100+ pre-built sections. Start with one area where current documentation feels most limiting, then expand as you become comfortable with the prompting process.