Writing great progress notes: when to use which template and why
For mental health professionals writing clinical documentation is essential.
It allows clinicians to track their client’s progress over time and provides a framework for consistent communication with other healthcare providers – including how a client is responding to treatment.
Mental health progress notes are also required for insurance purposes to prove that clients who cannot afford to pay out-of-pocket need to keep receiving therapy.
Notes that are written well, are more likely to help your clients. Not to mention, therapy progress notes document your competence as a therapist and help with any legal or billing disputes.
However, knowing which progress note template to use, and in which clinical context, is often challenging.
That’s why we’ve compiled an overview of the different progress note templates – and added real-world scenarios to show you which template to use and why.
The most frequently used progress note templates
The most frequently used progress notes are SOAP, DAP, BIRP, and GIRP.
Which patient progress note template do you use?
We’re often trained to use whatever our supervisor or agency does, without actually learning about which progress note template may be best suited to a particular modality or client situation.
And the truth is, that different progress notes are best for different things.
To make the right choice, it’s important to consider your area of specialty and the type of therapy you provide. And, in today’s world, you can also choose whether you’d like to use an AI-powered note-taking platform or not to save you time.
For a more in-depth review of the different templates with directions on what to include in each section, check out our SOAP, DAP, BIRP, and GIRP note articles.
Which progress note should you use and when?
The important commonalities between therapy progress notes aren’t something you have to worry about when making an individual template choice.
By documenting your session with any of the following progress note templates, you’ll be documenting treatment necessity and length, showcasing your competence, and keeping yourself to legal and ethical standards.
So, then, you might be asking, how do I choose between them? And what are the pros and cons of each? Read on to find out more or explore our psychotherapy vs. progress notes article.
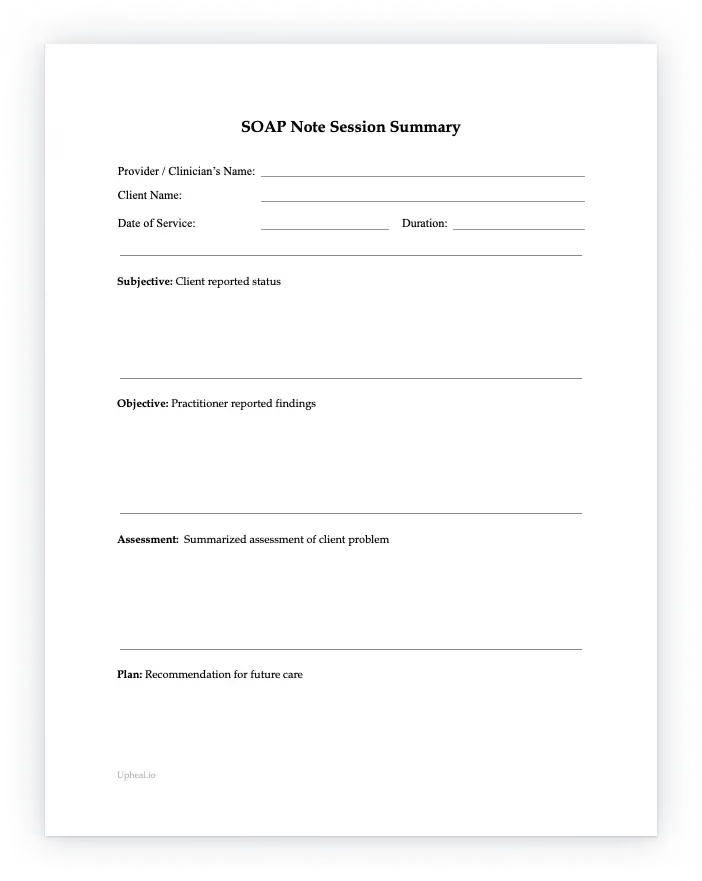
The SOAP note and its benefits
The SOAP note is the most commonly used progress note template, and most likely, the note your supervisor told you about.
It’s generally a favorite amongst therapists because it strikes a balance between capturing the important subjective and objective elements of a client's situation and is not reliant solely on the therapist's interpretation of the client's circumstance.
The essential components of a SOAP note are:
- The Subjective (S) section
Tracks the client’s subjective experience, feelings, and overall concerns. - The Objective (O) section
Comprised of the observable and measurable data collected during the appointment. - The Assessment (A) section
An important section that combines aspects of both Subjective and Objective observations and turns into the clinician's professional judgment and diagnosis. - The Plan (P) section
Goes over aspects of the next steps in the treatment plan, any necessary follow-ups, and homework items.
When to use a SOAP note template
- For complex clinical presentations - Because the SOAP template structure captures a more detailed client presentation case overall, it is helpful for complex cases with multiple factors or co-morbidities.
- For long-term therapy - SOAP note templates are great for tracking client progress over an extended period. Because the focus is on both the client's experience and yours, patterns are more easily identifiable allowing for treatment adjustment as needed.
- For situations requiring strict documentation - Some settings such as outpatient clinics, hospitals, or court-ordered clients require strict and detailed record keeping. The comprehensive nature of the SOAP note template is ideal for these situations.
Real-world scenario: the SOAP progress note template
The SOAP note template allows for a valuable contrast between the client’s and clinician’s observations.
First, the client’s Subjective POV is gathered. The client may report feeling “fine” which is added to the Subjective section including a quote about not understanding why family and friends “made them go to therapy”.
However, the clinician may observe a flat affect, lack of emotional response, slow moments, and other visible signs of depression in the Objective section.
They may justify a diagnosis of major depression in the Assessment section and finally, would discuss the use of CBT with homework exercises, aimed at reducing the depressive symptoms in the Plan section.
The DAP note and its benefits
The DAP structure is commonly used for clinical modalities that are short-term or more driven by solution-focused approaches to therapy.
The DAP format highlights the main problems in one data section which can be faster, and focuses on the practical solutions to solving these problems.
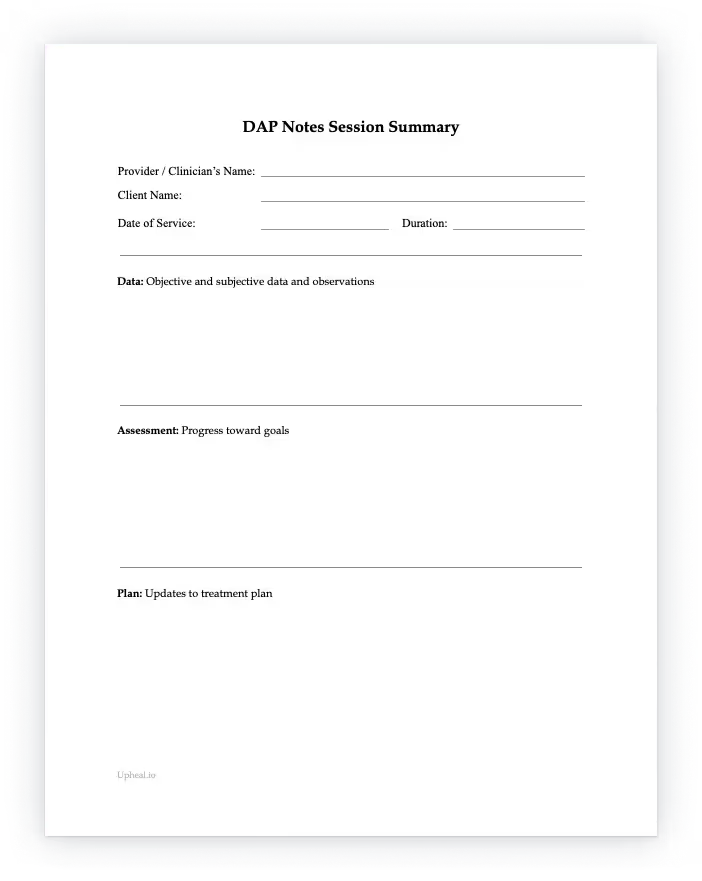
The essential components of a DAP note are:
- The Data (D) section
The “whats” of the session, including topics discussed and interventions used. Unlike in the SOAP note, all clincian-observed and client-reported symptoms are combined. - The Assessment (A) section
Documents the client’s emotional state during the session and represents the clinician’s interpretation of the data in the preceding section. Can include a diagnosis and any progress made towards treatment goals. - The Plan (P) section
Plans the next steps in the client's journey, including what you’d like them to do next and your own goals as their therapist.
When to use a DAP note template
- For therapists with a large caseload - DAP notes save time. They’re streamlined and efficient making them useful for therapists who see a high volume of clients.
- For a more client-centered approach to therapy - The DAP progress note template captures the client experience during the session in the Data and Assessment sections. This is helpful for therapists who want to prioritize the client's perspective over a more lengthy analysis as one would see in a SOAP note.
- Situations where discretion is key - Clients may present with severe trauma or other sensitive experiences. To maintain a safe and comfortable therapeutic space, at times, a DAP note is most helpful due to its concise and less intrusive nature.
- Collaborative care settings - Because the DAP note offers a clear and concise summary of the client's progress, it can be beneficial for multidisciplinary team settings with multiple providers.
Real-world scenario: the DAP progress note template
Details of this traumatic experience as shared with the therapist and the therapist’s decision to utilize a trauma-focused CBT intervention are all captured in the Data section.
The client's physical stress responses to recalling traumatic memories are then noted in the Assessment section along with the diagnosis.
Finally, the therapist sets an assignment – an “About You” trauma-focused CBT worksheet and documents this as part of the ongoing treatment planning for the client, making up the Plan section.
The BIRP note and its benefits
BIRP note templates are highly effective in therapy situations where the focus is on the client's behavior.
The overall emphasis is on specific targeted behaviors and the tracking of progress in modifying a client's behavior.
It’s especially useful for disorders where behavior is an important facet of the process, for example, OCD or Tourette’s. The sections that are included in this template are Behavior, Intervention, Response, and Plan.
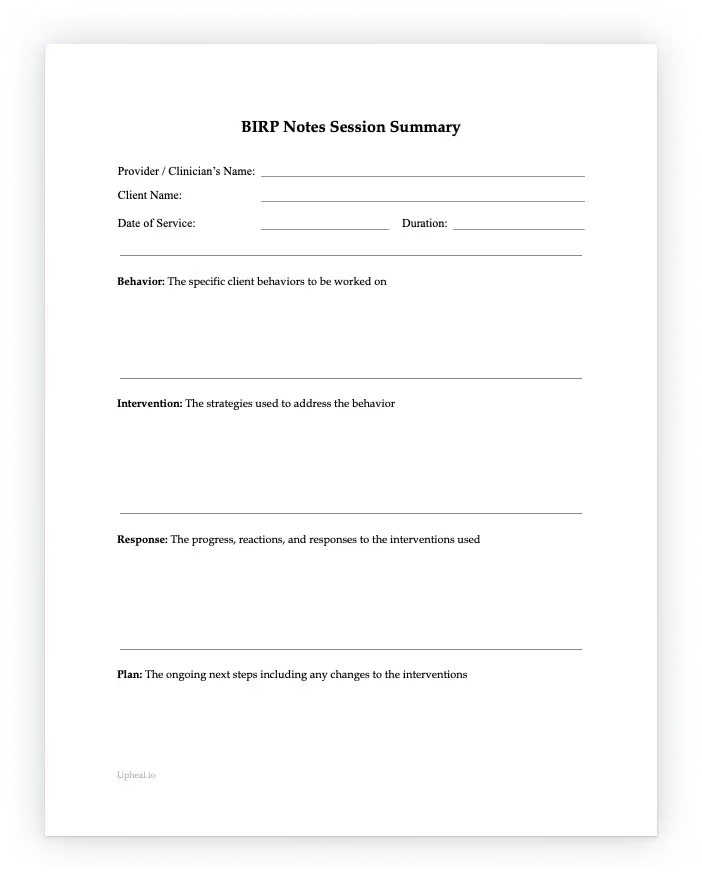
The essential components of a BIRP note are:
- The Behavior (B) section
Focuses on the client's specific behavior or behaviors that are noted in the session. - The Intervention (I) section
Where the strategies used to address the client's behavior will be recorded. - The Response (R) section
Documents any response the client has to the interventions used. - The Plan (P) section
Captures the ongoing next steps to manage the client's behavior.
When to use a BIRP note template
- Applied Behavioral Analysis (ABA)- ABA is rooted in the science of learning and behavior. ABA is commonly used with patients on the autism spectrum to improve skills and is also used in working with clients with developmental delays. The BIRP note template, with its emphasis on client behaviors, is a perfect fit for these settings.
- Treating children or adolescents with behavioral disorders - When treating children or teens with problematic behaviors, the BIRP note is perfect for highlighting the progress made concerning each of the targeted behaviors. As mentioned above, OCD can fit into this category.
- Working with couples and families - BIRP notes are very effective for tracking communication patterns and dynamics within a couple or family. The tracking of specific behaviors regarding these communication patterns helps to quickly identify areas of improvement in a couple or family unit.
- Substance use or eating disorder treatment - Therapists can track triggers, cravings, or compulsions and highlight relapse prevention strategies with ease using the BIRP progress note template.
- The application of specific skills - Such as relaxation skills, anger management, etc. Thanks to the focus on specific behavior or skills acquisition progress tracking, the BIRP note is ideal.
Real-world scenario: the BIRP template
The therapist will document the child's behavioral difficulty first – in this case, trouble focusing in the classroom for over 10 minutes. This will go into the Behavior section.
The therapist may then implement a token economy system for rewarding earned tokens for maintaining focus, which is an intervention and so will be documented in the Intervention section.
By the end of the week, the child's focus may have increased to 15 minutes a day. The therapist will document this in the Response section.
The therapist may also decide to continue the token system for the following week hoping to increase the time even more and this will be documented in the Plan section.
The GIRP note and its benefits
The GIRP template is most commonly used by therapists who employ goal‑oriented therapies such as motivational interviewing or Acceptance and Commitment Therapy (ACT).
This is because the unique feature of a GIRP note is its focus on the client's goal or desired outcome – making it a good choice for clients with a higher level of awareness and clarity.
The sections that are included in this template are Goals, Intervention, Response, and Plan.
The GIRP note can also be used for coaching since it describes exactly what the client wants to get out of sessions, whether that’s a long-term or short-term goal.
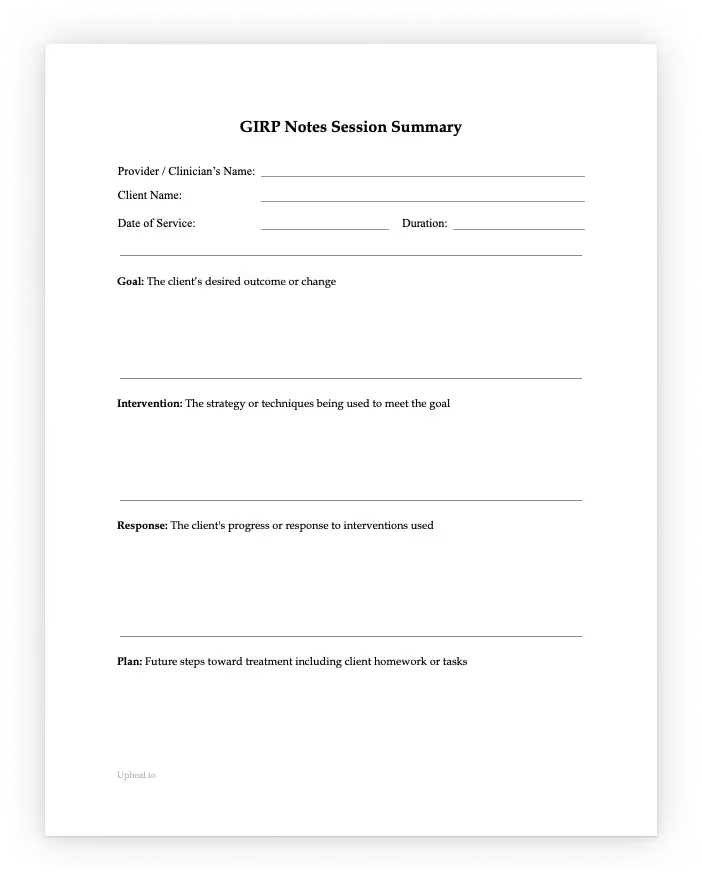
The essential components of a GIRP note are:
- The Goal (G) section
The desired outcome or change the client seeks, either short or long term. - The Intervention (I) section
The techniques, methods, or strategies the practitioner and client are using to work toward the desired change. - The Response (R) section
An objective account of the individual’s reaction or progress in response to the interventions used. This can help the clinician evaluate if the interventions they’re using are - The Plan (P) section
The plan sets out future steps, giving a clear roadmap for future treatment, services, and client homework or tasks, based on insights gained from the response to past interventions.
When to use a GIRP note template
- For clients resistant to change - Often, resistant clients can lack clear goals and this format can help the therapist and client clearly articulate the aim of therapy and track the progress toward agreed-upon goals. can be especially useful for resistant clients for whom.
- Life transitions - GIRP notes are useful to help manage transitions by setting small goals for motivation and confidence building that can help clients develop mastery of their situation. Examples include a career change, navigating through a divorce, or periods of intense grief.
- Brief interventions - The GIRP format is helpful in that it allows the therapist and client to set time-limited and focused goals. This is perfect for clients who need quick and targeted support.
- Group therapy - Overarching goals for a group as a whole, can be established using the GIRP template. At the same time, it can also be used to guide individuals within the group to create their own goals and work towards these goals for the resolution of unhelpful personal and group dynamics.
Real-world scenario: the GIRP template
If the goal is to reduce social avoidance by 50% in social settings, this would be documented in the Goals section.
The therapist discusses the use of mindfulness and relaxation practices in the session with the client; this is documented in the Intervention section.
When the client reports feeling fewer physical symptoms of anxiety in the role-play done in their session, the therapist documents this in the Response section.
Finally, the therapist assigns continued practice at a social gathering over the weekend as homework, and this is documented in the Plan section.
Concluding thoughts
If you've only ever been taught clinical documentation one way, we hope this article gave you helpful insight into the other documentation options available to you!
Making the right note choice can affect your therapeutic practice and while learning about them may be a little time-consuming at the start, it will help save you time in the long run especially once you know all about their intended use cases and benefits.
We recommend trying at least each of these once, to be better prepared for all kinds of clinical scenarios.
Focusing on particular therapy modalities and the notes best suited to them is also likely to help you feel more empowered when working with each client’s particular challenges.
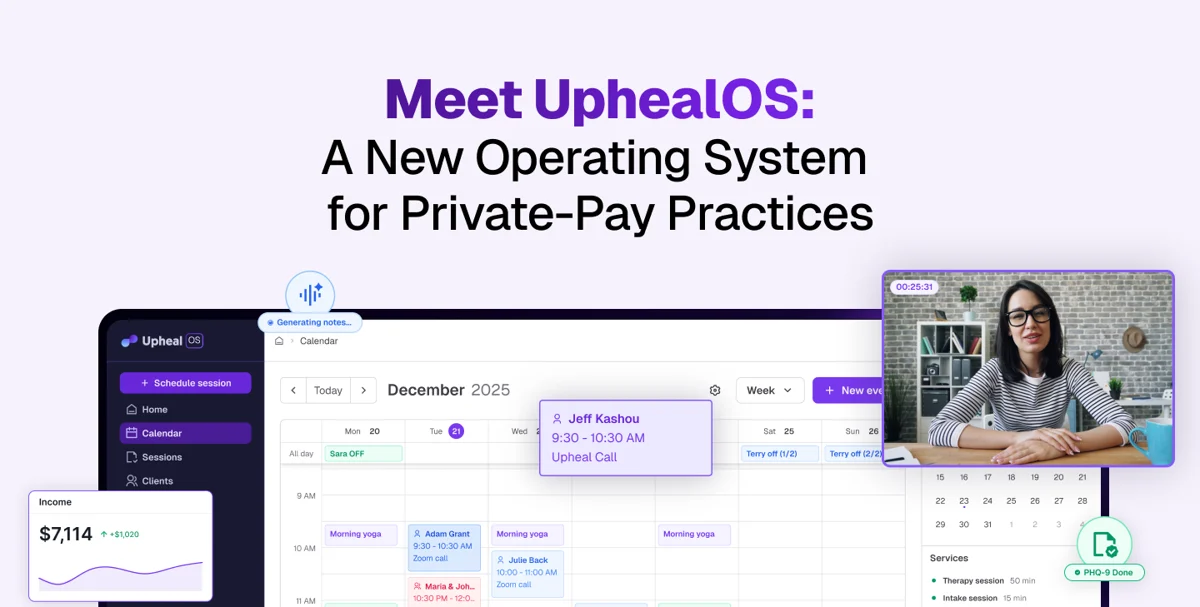
And of course, if you’re looking to save some important me or client time you can always try AI progress notes.
We recommend Upheal’s progress notes for both high-quality clinical insight and the variety of templates that are on offer. For a free trial of 15 sessions monthly, indefinitely, just sign up here.