How to Write SOAP Notes + Free Template and Example (2026)
SOAP Note Example / Template
Mental health professionals need to document client interactions for legal reasons, to help with the therapeutic process, and to justify the need for therapy to insurance companies on behalf of their clients.
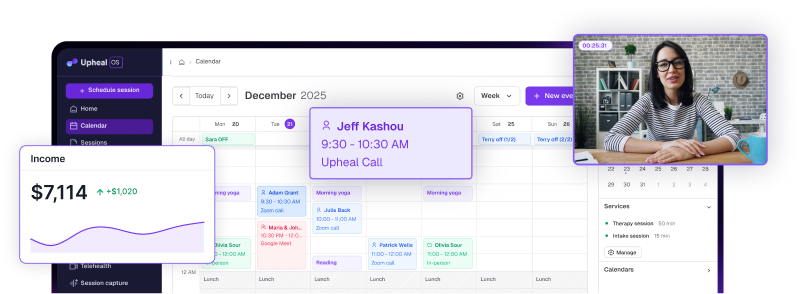
SOAP notes are just one example of the different progress note types that mental health professionals can use for their clinical documentation. SOAP notes are one of the most widely used formats for therapy documentation. Today, many clinicians are turning to AI SOAP notes to create accurate SOAP therapy notes faster, while reducing time spent on paperwork.
In this guide, you’ll learn what SOAP notes are, how to write effective SOAP therapy notes, and how to use a SOAP note template, including examples of how AI-generated SOAP notes work in practice. We’ll also provide a SOAP note example based on a real-life scenario, and an Upheal template that you can download for free.
What are SOAP notes in therapy?
SOAP notes are a standardized and concise way of capturing data from a client session including what the client is presenting with, their progress, and any future steps toward treatment.
SOAP notes are well-established in healthcare and are used by doctors, psychiatrists, nurses, therapists, psychologists, counselors, social workers, and more, to present a patient’s health findings in a clear and organized manner.
In mental health care, SOAP therapy notes help clinicians clearly document symptoms, progress, and treatment plans, and are increasingly created using AI SOAP note tools. Below is a SOAP note example from a member of our clinical team.
SOAP note therapy example
Here is an example from a real therapy scenario. How would you turn the following session into a mental health SOAP note?
In this case, the contrast between both the physical presentation of depressive symptoms and self-reported emotional experiences will be important to tracking CBT effectiveness and the progress of treatment.
Here is a SOAP note example. It's been written by our Head of Clinical Operations, Ted Faneuff, a licensed therapist, to make sure it's truly helpful to you.
Essential SOAP note components
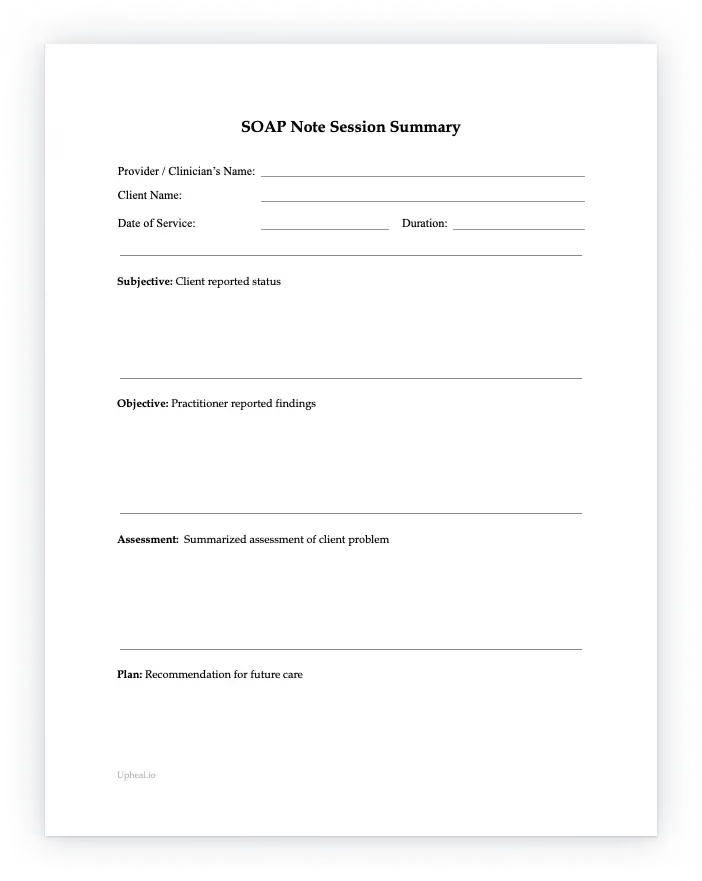
This SOAP note template is designed specifically for therapy SOAP notes and follows the same structure used by AI-generated SOAP notes, making it easy to switch between manual and automated documentation.
As you saw in the SOAP note example, each therapy SOAP note should carefully document the interaction between the client and the therapist and contain the Subjective, Objective, Assessment, and Plan sections.
Healthcare providers can then easily read and understand a client’s history, as can insurance companies.
- Subjective (S): Patient's stated experiences, feelings, and concerns.
- Objective (O): Observable and measurable data collected by the clinician.
- Assessment (A): Clinician's professional judgment and diagnosis.
- Plan (P): Treatment plan, follow-up, and next steps.
Free SOAP note template for therapy (PDF & Word)
Use our free SOAP note template for your clients sessions – it’s free to download.
5 common use cases (or when to use it)
Let’s look at the benefits of SOAP notes to help you identify when you should use the SOAP note template. Although each clinician is free to decide their preferred option, it can be helpful to learn about the benefits of each beforehand.
- It’s widely used in healthcare – Since the SOAP note is one of the most common note formats used across the healthcare sector, it’s a good choice if you know you’ll be working as part of a larger clinical team that involves members from different sectors.
- Unique contrast in points of view – The SOAP note is unique in that it contains both Subjective and Objective information, making it easy to separate self-reported Subjective client information from physical presentation and symptoms, providing an interesting and important contrast between the client’s view and the therapist’s.
- Better capture of complex clinical presentations - Because the SOAP template structure captures a more detailed client presentation case overall, it is helpful for complex cases with multiple factors or co-morbidities.
- Ideal for long-term therapy - SOAP note templates are great for tracking client progress over an extended period. Because the focus is on both the client's experience and yours, patterns are more easily identifiable allowing for treatment adjustment as needed.
- For situations requiring strict documentation - Some settings such as outpatient clinics, hospitals, or court-ordered clients require strict and detailed record keeping. The comprehensive nature of the SOAP note template is ideal for these situations.
What is the benefit of using soap notes?
- By using the above sections and tips, you’ll ensure compliance with clinical documentation standards.
- Sometimes clients say one thing with words, but their faces, tones of voice, and bodies tell an entirely different story.
- It will be easier for insurance companies to grant your client more sessions under your care.
- It’s easier to keep track of the important milestones happening for your client on their healing journey, and your therapeutic work, together.
- By using the SOAP note template, you’ll be able to share clinical documentation easily with medical professionals in other fields to help your client towards the best possible care.
How to write a SOAP note?
Each SOAP note contains four components: the Subjective, Objective, Assessment, and Plan sections. When writing your note, remember to choose the aspects of your session that are most relevant to your client, their treatment, and their healing journey.
Your note shouldn't be a contender for the next Harry Potter – it should be succinct yet exhaustive enough so that you, another clinician, and an insurance company can see what’s been addressed and how the therapy will continue.
The Subjective (S) section of a SOAP note
In this section, the goal is to capture the client’s subjective experiences, feelings, and concerns as reported by the client during your session.
It can also be a quote or short statement that describes why the patient is presenting to therapy or what they’ve been going through and for how long. When writing the Subjective section:
The Objective (O) section of a SOAP note
This section should include observable, quantifiable, and measurable data. In other words, externally visible information that anyone observing the session could agree to have seen.
It can also include certain categories of the MSE or Mental Status Exam such as orientation to time and place, speech and motor activity, thought processes, attitude, insight, and memory capacity.
The Assessment(A) section of a SOAP note
The Assessment section synthesizes the subjective and objective evidence to arrive at a diagnosis.
In addition, the Assessment section is an ongoing story of the client's progress, stagnation, or development with insight into the treatment’s efficacy. In other words, it should capture the development of the client’s progress in therapy.
The Plan (P) section of a SOAP note
The P section should cover the next course of action in the treatment plan for the client, even work or consultations with other healthcare professionals.
Make sure to focus on things both parties have agreed to. Summarize the next steps and any implementation details.
Tips for the SOAP writing process
- Allocating regular documentation time in your day – Too often therapists go from session to session and then have to play documentation catch-up in the evenings or on weekends. Maintain a buffer for documentation between client appointments. It’s good for your mental health too.
- Making a mental shift around charging for note time – It may not happen during a session, but writing progress notes is an essential part of the therapy process. Don’t forget to include this time in your hourly charge or service.
- Get into a routine with your pencil, tablet, or AI tool of choice – Once you’ve got your time and peace of mind, you can choose a range of ways to write your SOAP note. From taking notes in a notepad the old-fashioned way to using a tablet, EHR, or simply writing up what you remember post-session on your laptop – everyone has a different clinical documentation process. You can even use an AI platform like Upheal and let it run in the background.
- Change the order if you need – It has been found that it can be helpful to rearrange the order to form APSO. Assessment, Plan, Subjective, and Objective, presents the most relevant information to ongoing care at the beginning of the note, where it can be found quickly, shortening the time required for the clinician to find a colleague's assessment and plan. (National Library of Medicine: SOAP Notes, Vivek Podder; Valerie Lew; Sassan Ghassemzadeh.) But you do you!
- Go ahead and write the thing – Procrastination just makes us feel more and more under pressure. Let go of perfectionism, and do your best, one sentence at a time. That’s it!
Conclusion
Did you learn all you needed to know about the therapy SOAP note?
We hope so. We know that as a mental health provider, time is of the essence. And yet, you want to be sure you’re writing a perfect patient SOAP note that will help your clients and you!
We understand.
Hopefully, this guide and our SOAP note example provided you with all the information and motivation you need to know when to choose to write using the SOAP note template and all the benefits it can bring.
Please remember that you’re doing a tremendous service to the world – and hopefully, the faster and easier SOAP note writing can be, the more time you can spend on yourself and your clients.