Treatment plan for PTSD: A comprehensive clinical guide
With approximately 6% of adults experiencing PTSD at some point in their lives, and about 13 million Americans affected in any given year, post-traumatic stress disorder represents one of the most significant mental health challenges in clinical practice.
This guide demonstrates systematic approaches to PTSD treatment planning, including examples as a jumping-off point for time-strapped clinicians.
Example treatment plan for PTSD
I. Diagnosis
Getting the right diagnosis is about more than putting the right heading on your documentation.
Thoughtful differential diagnosis that takes into account the varied presentations of traumatic experiences, intrusive symptoms, and functional impairment allows you to deliver better care while avoiding audits, clawbacks, and denials.
Common ICD-10 codes for PTSD
Common diagnostic codes include:
- F43.10: Post-traumatic stress disorder, unspecified
- F43.11: Post-traumatic stress disorder, acute
- F43.12: Post-traumatic stress disorder, chronic
- F43.0: Acute stress reaction
- F43.8: Other reactions to severe stress
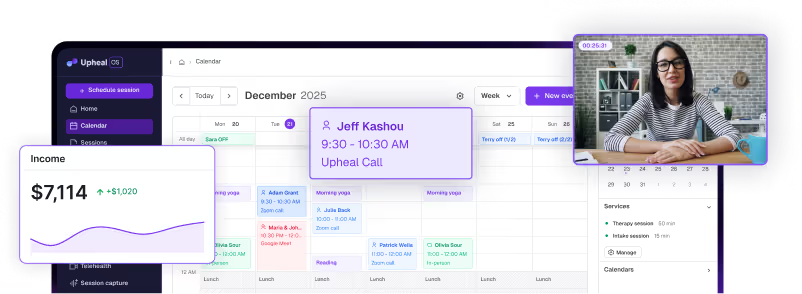
Upheal automatically suggests appropriate ICD-10 codes based on your session content and clinical documentation, reducing coding errors and ensuring compliance.
Accurate coding isn't just about reimbursement; it's about demonstrating medical necessity and maintaining your professional integrity.
Upheal’s Compliance Checker feature reviews your notes against established payer criteria, flagging potential issues before submission.
II. Presenting problems
Effective treatment planning begins with comprehensive assessment of presenting symptoms. Common presentations of PTSD include:
- Trauma-related re-experiencing: Recurrent intrusive memories, nightmares, flashbacks, or physiological reactions to trauma cues
- Persistent avoidance: Active avoidance of trauma-related thoughts, feelings, people, places, or situations
- Negative alterations in cognition and mood: Persistent negative beliefs about self or world, distorted blame, persistent negative emotional states, detachment from others
- Marked alterations in arousal and reactivity: Hypervigilance, exaggerated startle response, irritability, reckless behavior, concentration problems, sleep disturbance
- Dissociative symptoms: Depersonalization, derealization, or dissociative amnesia (in some cases)
- Functional impairments: Significant distress or impairment in social, occupational, or other important areas of functioning
- Comorbid conditions: Often co-occurring depression, anxiety disorders, substance use disorders, or suicidal ideation
III. Objectives
Research demonstrates that structured psychotherapy combined with clear, measurable objectives significantly improves PTSD treatment outcomes.
Effective treatment planning requires specific, measurable, achievable, relevant, and time-bound (SMART) objectives that demonstrate progress toward recovery.
Goal ideas for PTSD treatment
Symptom reduction goals:
- Decrease frequency and intensity of intrusive memories and flashbacks
- Reduce avoidance behaviors related to trauma triggers
- Improve sleep quality and duration
- Decrease hyperarousal symptoms
Cognitive restructuring goals:
- Challenge and modify trauma-related cognitive distortions
- Develop balanced perspectives about safety and trust
- Reduce self-blame and guilt
Functional restoration goals:
- Return to work or meaningful daily activities
- Rebuild social connections and support systems
- Re-engage in previously enjoyed activities
- Improve interpersonal relationships
Upheal's Golden Thread feature analyzes your session content and intake materials to automatically suggest clinically appropriate SMART goals.
These AI-generated objectives can be edited and customized to match your specific clinical approach, saving valuable planning time while ensuring comprehensive coverage of treatment domains.

IV. Interventions
For many therapists, articulating interventions proves surprisingly challenging.
The therapeutic work happens organically in session — those subtle moments when you help a client ground themselves during a flashback, or gently challenge a distorted belief about their trauma.
But translating these nuanced clinical moments into clear, insurance-appropriate language? That's where many of us struggle.
Common evidence-based interventions for PTSD
Trauma-focused interventions:
- Prolonged Exposure (PE) therapy
- Cognitive Processing Therapy (CPT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Narrative Exposure Therapy (NET)
- Written Exposure Therapy
Cognitive-behavioral approaches:
- Cognitive restructuring for trauma-related beliefs
- Behavioral activation for depressive symptoms
- Stress inoculation training
- Relaxation and grounding techniques
Stabilization and coping skills:
- Distress tolerance skills training
- Emotion regulation strategies
- Mindfulness-based interventions
- Safety planning and crisis management
Upheal's AI clinical notes capture the nuanced therapeutic work happening in your sessions, automatically translating clinical moments into professionally appropriate, modality-specific intervention language.
Common modalities for PTSD treatment
The most effective treatments for PTSD include:
- Cognitive Processing Therapy (CPT): A structured 12-session protocol focusing on challenging stuck points and cognitive distortions related to trauma
- Prolonged Exposure (PE): Systematic approach involving imaginal and in-vivo exposure to reduce avoidance and process traumatic memories
- Eye Movement Desensitization and Reprocessing (EMDR): Bilateral stimulation combined with trauma processing to reduce distress associated with traumatic memories
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): Particularly effective for children and adolescents, combining cognitive, behavioral, and family therapy approaches
Additional supportive modalities may include:
- Narrative Exposure Therapy (NET)
- Brief Eclectic Psychotherapy
- Present Centered Therapy
- Skills Training in Affective and Interpersonal Regulation (STAIR)
V. Progress monitoring
Continuous monitoring ensures treatment effectiveness and provides crucial documentation for insurance — namely, justification of medical necessity.
For PTSD treatment, careful tracking of symptom reduction and functional improvement demonstrates the value of ongoing therapy while maintaining compliance standards.
Common ways to measure progress in PTSD treatment
Standardized assessment tools:
- PTSD Checklist for DSM-5 (PCL-5)
- Clinician-Administered PTSD Scale (CAPS-5)
- Impact of Event Scale-Revised (IES-R)
- PTSD Symptom Scale Interview (PSSI-5)
Functional metrics:
- Sleep quality and duration tracking
- Social engagement frequency
- Work/school attendance and performance
- Substance use monitoring
Symptom tracking:
- Frequency and intensity of flashbacks/nightmares
- Avoidance behaviors
- Hyperarousal symptoms
- Dissociative experiences
Upheal's Golden Thread features automatically weave consistent narratives of medical necessity throughout your documentation.

From treatment plans to progress notes, our AI ensures each piece of documentation builds upon previous sessions, clearly demonstrating therapeutic progress and maintaining compliance standards.
This integrated approach eliminates documentation gaps that can trigger insurance reviews while providing clinicians with comprehensive client progress visualization.
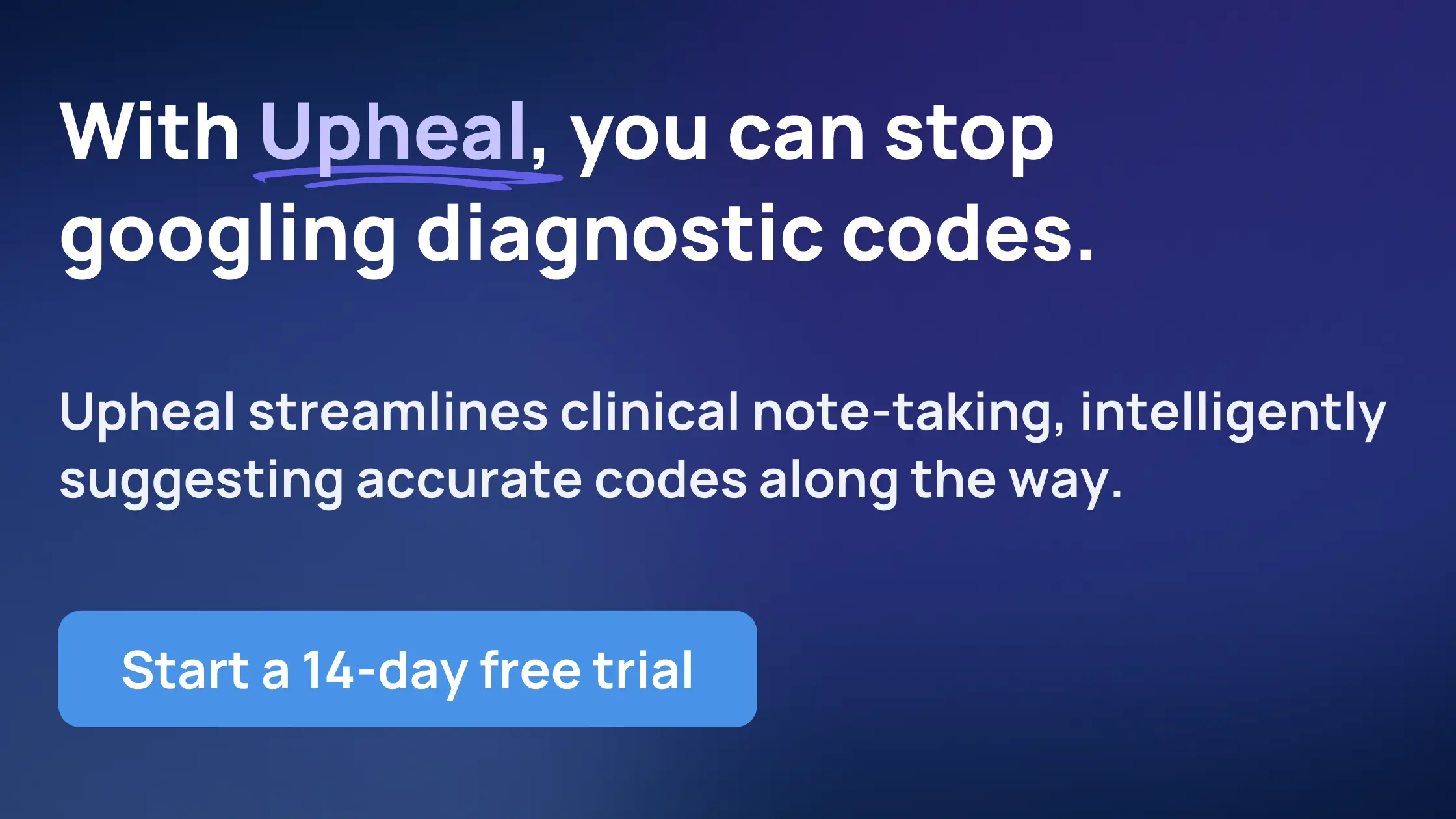
Write your best treatment plans
Ready to transform your clinical documentation?
Upheal's intelligent platform streamlines your clinical workflow while maintaining the highest standards of care.
Our purpose-built features for trauma treatment help you focus on what matters most — your clients' recovery journey.
Start your free 14-day trial today and discover how intelligent documentation can enhance your clinical practice.