Compassion fatigue test: Are you putting your own oxygen mask on first?

Compassion is our superpower, but a costly one
In helping professions like therapy, coaching, social work, or healthcare, compassion isn’t just a nice-to-have skill; it’s essential. The ability to show up with empathy, to sit with another’s pain, is what allows healing to happen.
But over time, the very qualities that make you effective can also leave you vulnerable.
This phenomenon is known as compassion fatigue. It is the negative effect that long-term caring for those in distress has on a person’s ability to feel compassion for others (Figley, 1995). In helping professions, over time, it can lead to a gradual depletion of empathy and a reduced ability to nurture others (Adams et al., 2006).
In fact, research has shown that nearly 46% of counselors experience compassion fatigue at some point in their careers. That’s almost half!
Recognizing the signs early is critical not only for your own well-being but also for the quality of care you provide.
In the first part of this blog, we’ll explore markers of compassion fatigue to see if you’re at risk. And the second, we’ll share our tips for how to protect your capacity for care without burning out (using the research).
Let’s evaluate how at risk you may be
Research shows that several factors have been found to contribute to compassion fatigue. If you’re reading this article, chances are you may be at risk. Why don’t you take a few minutes and mentally check off how many of the below you experience daily? Then, we’ll delve right into the symptoms of compassion fatigue.
- Do you work in isolation? Without the support of peers or supervisors to debrief and share challenges, you might feel alone in your struggles, which can exacerbate the fatigue.
- Do you feel solely responsible for client outcomes? When you carry the weight of your clients' progress on your shoulders, it can easily lead to stress and self-doubt.
- Do you over-identify with the client? This kind of deep, empathic merging is different from countertransference, which typically stems from unresolved patterns from our own early relationships (Figley, 2002). In over-identification, it’s the excess empathy itself, without clear emotional boundaries, that begins to cause distress and exhaustion.
- Can you separate your distress from the client’s? If your work involves supporting trauma survivors, you may be especially vulnerable to secondary trauma, i.e., the indirect exposure to the pain of others. When discussing the vivid descriptions of traumatic events with clients, it can leave an imprint, leading to symptoms that mirror PTSD. Pearlman and Saakvitne (1995) described this as vicarious traumatization i.e., a gradual process where the weight of bearing witness begins to impact how you see yourself, your clients, and the world.
- Do you have doubts about “doing enough”? Constantly questioning whether you’re doing enough can lead to emotional exhaustion, as it places an unrealistic burden on yourself.
How many did you answer yes to? The more of these risk factors you can relate to in your daily practice, the higher your risk of compassion fatigue. Thankfully, you can read on further to find out how to manage if you do find yourself experiencing the signs. And don’t worry, there is definitely something you can do!
When helping hurts – how to know if you have compassion fatigue
Unfortunately, there’s another side to compassion. Compassion fatigue can quietly build up even when we are deeply committed to our clients' healing. Every therapist’s pathway to compassion fatigue can look different, but some common contributors can provide insight into what might be at play.
If you’re working harder than usual and feeling off, these signs may indicate that you’re experiencing compassion fatigue:
- Loss of empathy: a growing detachment from your clients, making it hard to engage in the compassionate presence that you once provided in sessions
- Physical, emotional, and cognitive symptoms in your daily life: trouble sleeping, irritability, anxiety, hypervigilance, and a general diminished interest in activities you once enjoyed (Figley, 1995),
- Impaired executive functioning that isn’t normally experienced, which can mean things like difficulty thinking clearly or making decisions (Stoewen, 2020)
- A growing sense of detachment or numbness in your approach to clients.
These symptoms can coexist with depression or anxiety, but compassion fatigue is unique because of the context it arises in (caring for others). Therefore, these shouldn’t be general symptoms throughout one’s life. A key marker to watch for is a growing sense of detachment or numbness, especially within the therapeutic relationship itself.
It can be easy to confuse compassion fatigue with burnout, but they aren't quite the same. While burnout is about being worn down by work demands in general, compassion fatigue is specifically tied to the relational and emotional work of caring for others. Compassion fatigue often comes first in caregiving professions—it’s the emotional residue from bearing witness to trauma over and over again. If unaddressed, it can lead to burnout, which is a broader state of emotional, physical, and mental exhaustion from chronic stress.
Holding space — but not the whole universe
Providing a safe space for clients is one of the most important parts of the job. Yet, it’s a skill that perhaps should be taught in graduate schools with an asterisk: creating that space should not come at the cost of your own well-being.
When compassion fatigue sets in, it can subtly erode the quality of care you offer. It may show up as difficulty attuning to a client’s needs, challenges in examining their experiences without bias, or trouble engaging in core therapeutic techniques like reflective listening. Over time, this can negatively impact clinical outcomes and the therapeutic alliance you work so hard to build.
Outside of the therapy room, it can have spillover effects into your personal life, increasing the risk of burnout. When left unrecognized for too long, it can result in self-contempt, low job satisfaction, and psychosomatic problems (Demerouti et al., 2000).
It can even create an internal tug of war of wanting to do the best at your job, and being struck with the guilt of not being “able” to do enough. Acknowledging this dynamic isn’t a weakness, it’s an act of professional responsibility and self-compassion. The good news is that the earlier we identify the signs and risk factors for compassion fatigue, the more we can take active steps to mitigate its impact or prevent it in the first place.
Caring for yourself while caring for others
While compassion fatigue may be inevitable in certain contexts, the good news is that with the right attention, it can often be managed and/or prevented. There are a plethora of ways to address compassion fatigue, and you can choose the ones that resonate most with you and fit with your unique circumstances.
Here are some strategies to consider or experiment with:
- Self-monitoring and self-care: As you are preaching the importance of self-care to your clients, remember to practice it yourself, too. Research shows that it can significantly reduce the likelihood of compassion fatigue (Rokach & Boulazreg, 2020)
- Micro-moments of restoration: Small actions like a few minutes of breathwork, grounding exercises, or stepping outside for fresh air between sessions can create powerful resets. We also recognize that it can be difficult to incorporate these practices with busy schedules, and so you could:
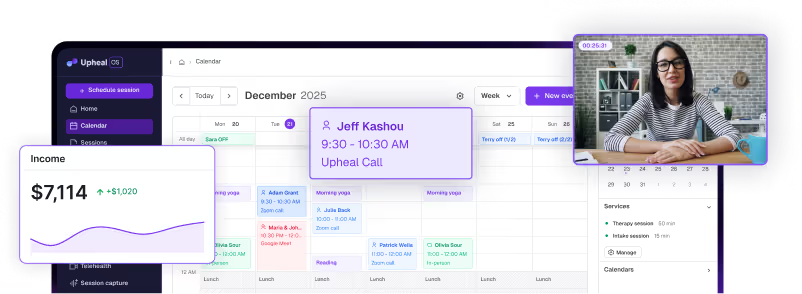
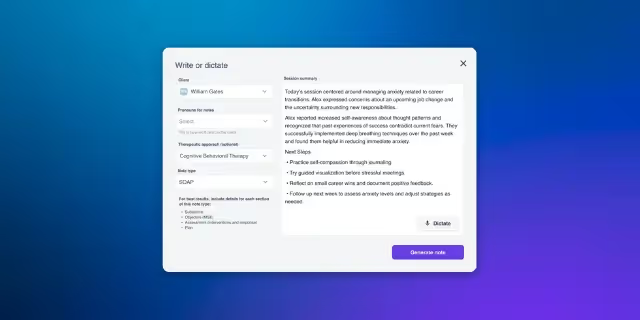
- Use Upheal’s session analytics (talking ratio and speech cadence) to dive deeper into subtle shifts in your own talk time and emotional engagement. These can potentially serve as early signs of you feeling depleted.
- Use Upheal to take notes during the session, so that you have some time between sessions for self-care, and it is easy to incorporate those micro-moments of restoration
- Use Upheal’s session analytics (talking ratio and speech cadence) to dive deeper into subtle shifts in your own talk time and emotional engagement. These can potentially serve as early signs of you feeling depleted.
- Participate in supervision or peer consultation: Formal or informal supervision can help you process emotional material while maintaining healthy emotional boundaries with clients (Vu & Bodenmann, 2017).
- Engage in your own therapy: You know better than anyone that personal therapy can provide a safe space to process the emotional demands of clinical work and strengthen resilience. Having an outlet for particularly emotionally draining cases can help you release professional tension before stepping into your personal life.
- Review and adjust your caseload: While you may feel tempted to help every client referred to you, learning to say “no” with compassion to yourself and to others is vital. If you have control over the number and/or type of cases you see, you may be able to make adjustments to allow for a more sustainable caseload.
- Lean into your support system: Regularly connect with peers, mentors, or loved ones who can offer perspective and encouragement.
- Switch up the flow: Adding non-clinical activities—like writing, research, curriculum design, mentoring, or consulting—into your week can offer a cognitive and emotional reset, helping break the drain of back-to-back therapy sessions. Diversifying your workday keeps things stimulating and can reduce the emotional wear-and-tear that comes from continuous therapeutic engagement.
Hold space for yourself, too
To provide effective care, it is important to check in with ourselves as well. The earlier you can recognize when your system is feeling overloaded or dysregulated, the better you can protect both your personal and professional life from the fallout. Stepping back from work or reducing your caseload isn’t a sign of weakness; it’s a sign that you’re honoring the very human limits of your own nervous system.
The term “empathy fatigue,” coined by Dr. Mark Stebnicki, reinforces that these feelings are not avoidable, given the nature of our work.
It would be unnatural to expect ourselves to continually hold space for others without feeling the weight of it. In those moments when fatigue or distraction creeps in, try practicing mindful self-compassion. Acknowledge that it's okay to feel worn down. Gently bring your attention back, without judgment, just as you would guide a client. You don’t have to outrun compassion fatigue. You simply have to recognize it and respond with the same care you extend to everyone else.
“You can’t pour from an empty cup — but you also don’t need to wait until it’s empty to refill it.”
Resources for managing compassion fatigue
Experiencing compassion fatigue is simply a human response to repeated exposure to suffering, one that even counselors are not immune to. The most important thing to remember is to act fast once you notice that it’s happening.
If you’re interested in learning more or finding ways to manage compassion fatigue, here are some excellent resources to explore:
- Compassion Fatigue Awareness Project: This website offers a wealth of information on understanding and addressing compassion fatigue. It also provides tools and workshops designed to help caregivers, mental health professionals, and anyone working in high-stress environments.
- YouTube Video: Understanding Compassion Fatigue: Watch this insightful video that delves into the causes and impacts of compassion fatigue, offering practical advice on how to recognize it and take steps to manage it effectively.
Note: this article should not be taken as clinical advice.