Treatment plan for depression: A comprehensive clinical guide

Depression affects millions of people worldwide, making it one of the most prevalent mental health conditions clinicians encounter.
For therapists pressed for time but committed to delivering exceptional care, having a clear treatment plan framework can transform both clinical outcomes and documentation efficiency.
This comprehensive guide provides evidence-based strategies and practical examples to help you develop effective treatment plans for depression while maintaining compliance with insurance requirements.
Example treatment plan for depression
I. Diagnosis
Getting the right diagnosis goes beyond putting the correct heading on your documentation.
Thoughtful differential diagnosis that considers the varied presentations of depression, its episodic nature, and comorbid conditions enables you to deliver superior care while avoiding audits, clawbacks, and denials.
The importance of well-considered differential diagnosis cannot be overstated.
Depression-focused psychotherapy is typically considered the initial treatment method for mild to moderate MDD, with cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT) showing significant clinical evidence.
Accurate coding ensures proper treatment planning and reduces insurance complications.
Common ICD-10 codes for depression
Common diagnostic codes for depression include:
- F32.0: Major depressive disorder, single episode, mild
- F32.1: Major depressive disorder, single episode, moderate
- F32.9: Major depressive disorder, single episode, unspecified
- F33.0: Major depressive disorder, recurrent, mild
- F33.1: Major depressive disorder, recurrent, moderate
- F33.2: Major depressive disorder, recurrent, severe without psychotic features
- F33.3: Major depressive disorder, recurrent, severe with psychotic features
- F33.9: Major depressive disorder, recurrent, unspecified
Accurate coding isn't just about reimbursement — it's about demonstrating medical necessity and maintaining your professional integrity.
Well-considered differential diagnosis helps distinguish between different types of depressive disorders and rules out medical conditions that might present with similar symptoms.
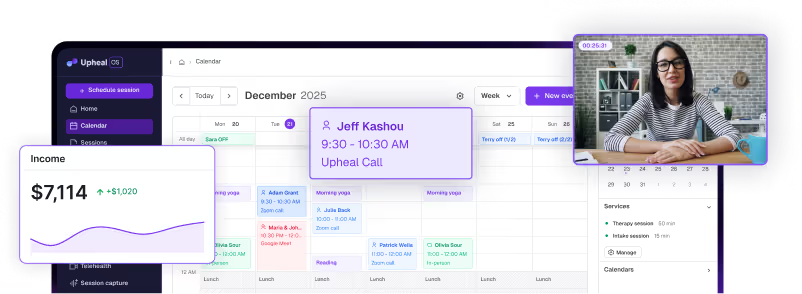
Upheal automatically suggests appropriate ICD-10 codes based on your session content and clinical documentation, reducing coding errors and ensuring compliance.
The risk of clawbacks, denials, and audit issues significantly increases when coding lacks precision. Insurance payers increasingly scrutinize claims, making accurate documentation essential for maintaining practice sustainability.
Upheal's Compliance Checker feature reviews your notes against established payer criteria, flagging potential issues before submission to mitigate the risk of clawbacks, denials, and audit issues.
II. Presenting problems
Effective treatment planning begins with comprehensive assessment of presenting symptoms. Common presentations of depression include:
- Persistent depressed mood: Feelings of sadness, emptiness, or hopelessness that persist most of the day, nearly every day
- Anhedonia: Markedly diminished interest or pleasure in all, or almost all, activities
- Significant weight changes: Unintentional weight loss or gain, or changes in appetite
- Sleep disturbances: Insomnia or hypersomnia nearly every day
- Psychomotor symptoms: Agitation or retardation observable by others
- Fatigue or energy loss: Nearly every day, affecting daily functioning
- Feelings of worthlessness: Excessive or inappropriate guilt, often unrealistic
- Concentration difficulties: Diminished ability to think, concentrate, or make decisions
- Suicidal ideation: Recurrent thoughts of death or suicide, with or without specific plans
- Functional impairment: Significant distress or impairment in social, occupational, or other important areas
- Interpersonal difficulties: Social withdrawal, relationship conflicts, or challenges maintaining connections
III. Objectives
Research demonstrates that structured psychotherapy significantly improves depression treatment outcomes when combined with clear, measurable objectives.
Based on significant clinical evidence, cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT) are recommended as first-line psychotherapeutic approaches.
Effective treatment planning requires specific, measurable, achievable, relevant, and time-bound (SMART) objectives that demonstrate progress toward recovery.
Goal ideas for depression treatment
Symptom reduction goals:
- Decrease frequency and intensity of depressive episodes
- Improve sleep quality and duration
- Increase energy levels and motivation
- Reduce negative self-talk and rumination
Behavioral activation goals:
- Re-engage in previously enjoyed activities
- Establish consistent daily routines
- Increase social interactions and connections
- Improve self-care practices
Cognitive restructuring goals:
- Challenge and modify negative thought patterns
- Develop balanced perspectives about self and situations
- Reduce all-or-nothing thinking
- Improve problem-solving skills
Functional restoration goals:
- Return to baseline work or academic performance
- Rebuild and maintain relationships
- Increase participation in meaningful activities
- Improve overall quality of life
Upheal's Golden Thread feature analyzes your session content and intake materials to automatically suggest clinically appropriate SMART goals.
These AI-generated objectives can be edited and customized to match your specific clinical approach, saving valuable planning time while ensuring comprehensive coverage of treatment domains.

IV. Interventions
For clinicians, it's common to experience a kind of intervention blindness.
Therapeutic work happens organically in session, but articulating those interventions clearly in documentation proves challenging.
Thoughtfully planning interventions from the beginning of treatment helps you maintain treatment plan integrity while making it easier to describe what you're doing in each session.
Common evidence-based interventions for depression
Cognitive-behavioral approaches:
- Cognitive restructuring for negative thought patterns
- Behavioral activation to counter withdrawal and anhedonia
- Problem-solving training for daily challenges
- Relapse prevention planning
Interpersonal approaches:
- Interpersonal therapy (IPT) for relationship difficulties
- Communication skills training
- Grief and loss processing
- Role transition support
Mindfulness-based interventions:
- Mindfulness-based cognitive therapy (MBCT)
- Acceptance and commitment therapy (ACT) techniques
- Present-moment awareness practices
- Value-based action planning
Supportive interventions:
- Psychoeducation about depression and treatment
- Safety planning for suicidal ideation
- Crisis intervention strategies
- Family therapy or support involvement
Upheal's AI clinical notes capture the nuanced therapeutic work happening in your sessions, automatically translating clinical moments into professionally appropriate, modality-specific intervention language.
Common modalities for depression treatment
The most effective treatments for depression are well-established in research literature.
Depression-focused psychotherapy is typically considered the initial treatment method for mild to moderate MDD, with cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT) showing the strongest evidence base.
- Cognitive Behavioral Therapy (CBT): CBT addresses the interconnected relationship between thoughts, feelings, and behaviors. This structured approach helps clients identify and modify negative thought patterns while engaging in behavioral changes that improve mood and functioning.
- Interpersonal Therapy (IPT): IPT focuses on improving interpersonal relationships and communication patterns to help relieve symptoms. It addresses four main problem areas: grief, role disputes, role transitions, and interpersonal deficits.
- Behavioral Activation (BA): BA specifically targets the behavioral symptoms of depression by systematically increasing engagement in meaningful, pleasurable, and goal-oriented activities.
- Mindfulness-Based Cognitive Therapy (MBCT): MBCT combines cognitive therapy techniques with mindfulness practices to help prevent relapse by teaching clients to recognize and disengage from negative thought patterns.
Additional evidence-supported modalities include:
- Acceptance and Commitment Therapy (ACT)
- Dialectical Behavior Therapy (DBT) skills training
- Problem-Solving Therapy (PST)
- Psychodynamic therapy for depression
V. Progress monitoring
Continuous monitoring ensures treatment effectiveness and provides crucial documentation for insurance — namely, justification of medical necessity.
In 2025, precision psychiatry approaches are revolutionizing depression treatment through personalized, data-driven monitoring that tailors treatment to each patient's unique biological and genetic makeup.
For depression treatment, careful tracking of symptom reduction and functional improvement demonstrates the value of ongoing therapy while maintaining compliance standards.
Common ways to measure progress in depression treatment
Standardized assessment tools:
- Patient Health Questionnaire-9 (PHQ-9)
- Beck Depression Inventory-II (BDI-II)
- Hamilton Depression Rating Scale (HAM-D)
- Generalized Anxiety Disorder-7 (GAD-7) for comorbid anxiety
Functional metrics:
- Sleep quality and duration tracking
- Activity level and engagement monitoring
- Social interaction frequency
- Work or academic performance indicators
Behavioral tracking:
- Completion of behavioral activation tasks
- Use of coping strategies
- Medication adherence (when applicable)
- Session attendance and engagement
Symptom monitoring:
- Mood ratings and fluctuations
- Suicidal ideation screening
- Energy levels and motivation
- Cognitive functioning improvements
Upheal's Golden Thread features automatically weave consistent narratives of medical necessity throughout your documentation.

From treatment plans to progress notes, our AI ensures each piece of documentation builds upon previous sessions, clearly demonstrating therapeutic progress and maintaining compliance standards.
This integrated approach eliminates documentation gaps that can trigger insurance reviews while providing clinicians with comprehensive client progress visualization.
Write your best treatment plans
Ready to transform your depression treatment documentation?
Upheal's intelligent platform streamlines your clinical workflow while maintaining the highest standards of care.
Our purpose-built features for depression treatment help you focus on what matters most — your clients' recovery journey.
- Save time: Reclaim hours spent on documentation with AI-powered treatment plan generation
- Ensure compliance: Reduce audit risk with documentation that meets payer standards
- Improve outcomes: Focus more on therapy, less on paperwork
- Maintain quality: Professional-grade documentation that reflects your clinical expertise
Start your free 14-day trial today and discover how intelligent documentation can enhance your clinical practice while supporting better outcomes for clients with depression.









![5 best AI scribes for therapists [2025]](https://cdn.prod.website-files.com/6328c07d72b05347cc236c49/68a793de80a95d779e3f6814_best%20ai%20scribe%20for%20therapists%20thumbnail.avif)
