Treatment plan for anxiety: A comprehensive clinical guide

Anxiety disorders represent the most common category of mental health conditions, affecting approximately 40 million adults in the United States each year.
This comprehensive guide demonstrates systematic approaches to anxiety disorder treatment planning, providing practical examples and evidence-based strategies for time-strapped clinicians who want to deliver exceptional care while maintaining compliance.
Example treatment plan for anxiety
I. Diagnosis
Getting the right diagnosis is about more than putting the right heading on your documentation.
Thoughtful differential diagnosis that takes into account the varied presentations of anxiety disorders, their episodic nature, and comorbid conditions allows you to deliver better care while avoiding audits, clawbacks, and denials.
Common ICD-10 codes for anxiety disorders
The most frequently used diagnostic codes include:
- F41.1: Generalized anxiety disorder
- F41.0: Panic disorder [episodic paroxysmal anxiety]
- F40.10: Social phobia, unspecified
- F41.3: Other mixed anxiety disorders
- F41.9: Anxiety disorder, unspecified
Accurate coding isn't just about reimbursement — it's about demonstrating medical necessity and maintaining your professional integrity.
Well-considered differential diagnosis helps distinguish between different types of anxiety disorders and rules out medical conditions that might present with similar symptoms.
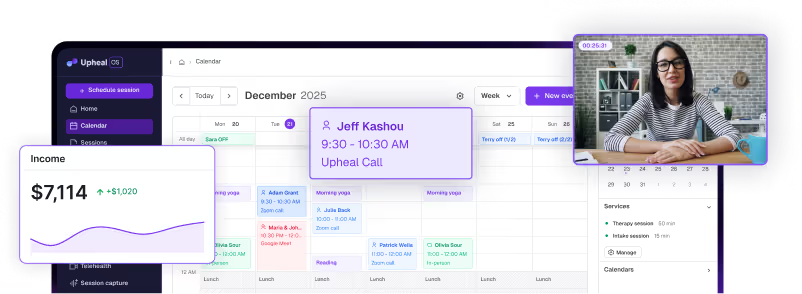
Upheal automatically suggests appropriate ICD-10 codes based on your session content and clinical documentation, reducing coding errors and ensuring compliance.
Upheal's Compliance Checker feature reviews your notes against established payer criteria, flagging potential issues before submission to mitigate the risk of clawbacks, denials, and audit issues.
II. Presenting problems
Effective treatment planning begins with comprehensive assessment of presenting symptoms. Common presentations of anxiety disorders include:
- Excessive worry or fear: Persistent, uncontrollable worry that is disproportionate to the actual threat or situation
- Physical symptoms: Muscle tension, restlessness, fatigue, rapid heartbeat, sweating, trembling, or gastrointestinal issues
- Cognitive symptoms: Racing thoughts, difficulty concentrating, mind going blank, or catastrophic thinking patterns
- Behavioral changes: Avoidance of feared situations, safety behaviors, procrastination, or compulsive checking
- Sleep disturbances: Difficulty falling asleep, staying asleep, or restless sleep due to anxious thoughts
- Social impairment: Withdrawal from social activities, relationships, or work responsibilities
- Panic symptoms: Sudden episodes of intense fear with physical symptoms like chest pain, shortness of breath, or dizziness
- Perfectionism: Excessive concern with making mistakes or not meeting unrealistic standards
III. Objectives
Research demonstrates that structured psychotherapy significantly improves anxiety treatment outcomes when combined with clear, measurable objectives.
Effective treatment planning requires specific, measurable, achievable, relevant, and time-bound (SMART) objectives that demonstrate progress toward recovery.
Goal ideas for anxiety treatment
Symptom reduction goals:
- Decrease frequency and intensity of worry episodes
- Reduce physical anxiety symptoms through relaxation techniques
- Improve sleep quality and duration
- Decrease avoidance behaviors
Cognitive restructuring goals:
- Challenge and modify catastrophic thought patterns
- Develop balanced perspectives about perceived threats
- Reduce "what-if" thinking and rumination
Functional restoration goals:
- Return to baseline work or academic performance
- Rebuild social connections and activities
- Increase participation in previously enjoyed activities
- Improve decision-making confidence
Upheal's Golden Thread feature analyzes your session content and intake materials to automatically suggest clinically appropriate SMART goals.

These AI-generated objectives can be edited and customized to match your specific clinical approach, saving valuable planning time while ensuring comprehensive coverage of treatment domains.
IV. Interventions
For many therapists, articulating interventions proves surprisingly challenging.
The therapeutic work happens organically in session — those moments when you help a client recognize their worry spiral, or gently guide them through a grounding exercise during a panic attack.
But translating these nuanced clinical moments into clear, insurance-appropriate language? That's where many of us struggle.
Thoughtfully planning interventions from the beginning of treatment can help you hold the treatment plan with integrity, while making it easier to describe what you're doing in each session.
Common evidence-based interventions for anxiety disorders
Cognitive-behavioral techniques:
- Cognitive restructuring for catastrophic thinking patterns
- Behavioral activation to counter avoidance
- Exposure therapy for phobias and panic disorder
- Relaxation training and stress management
Specialized approaches:
- Acceptance and Commitment Therapy (ACT) for emotion regulation
- Anxiety Release Protocol (ARP)
- Mindfulness-based interventions for present-moment awareness
- Exposure and Response Prevention (ERP) for anxiety-driven behaviors
Stabilization techniques:
- Grounding and distress tolerance skills
- Sleep hygiene education and implementation
- Safety planning for severe anxiety or panic
- Psychoeducation about anxiety physiology
Upheal's AI clinical notes capture the nuanced therapeutic work happening in your sessions, automatically translating clinical moments into professionally appropriate, modality-specific intervention language.
Psychotherapy modalities for anxiety
The most effective treatments for anxiety disorders are well-established in the research literature:
- Cognitive Behavioral Therapy (CBT): CBT can be regarded as the psychotherapy with the highest level of evidence for anxiety disorders. This structured approach addresses the interconnected relationship between thoughts, feelings, and behaviors.
- Acceptance and Commitment Therapy (ACT): ACT focuses on six processes through which an individual learns how to stay in the present, identify what is important to them, and engage in behavioral experiments to act out their values.
- Exposure Therapy: Exposure and Response Prevention (ERP) is the most critical component of effective cognitive behavioral treatment for anxiety disorders, particularly for phobias and panic disorder.
- Additional evidence-based modalities:
- Mindfulness-Based Stress Reduction (MBSR)
- Dialectical Behavior Therapy (DBT) skills training
- Interpersonal Therapy (IPT) for anxiety with interpersonal triggers
V. Progress monitoring
Continuous monitoring ensures treatment effectiveness and provides crucial documentation for insurance — namely, justification of medical necessity.
For anxiety treatment, careful tracking of symptom reduction and functional improvement demonstrates the value of ongoing therapy while maintaining compliance standards.
Common ways to measure progress in anxiety treatment
Standardized assessment tools:
- Generalized Anxiety Disorder-7 (GAD-7) scale
- Beck Anxiety Inventory (BAI)
- Hamilton Anxiety Rating Scale (HAM-A)
- Penn State Worry Questionnaire (PSWQ)
Functional metrics:
- Sleep quality and duration tracking
- Social engagement frequency
- Work or academic performance indicators
- Use of safety behaviors or avoidance patterns
Symptom tracking:
- Frequency and intensity of worry episodes
- Physical anxiety symptoms
- Panic attack frequency and severity
- Successful use of coping strategies
Upheal's Golden Thread features automatically weave consistent narratives of medical necessity throughout your documentation.

From treatment plans to progress notes, our AI ensures each piece of documentation builds upon previous sessions, clearly demonstrating therapeutic progress and maintaining compliance standards.
This integrated approach eliminates documentation gaps that can trigger insurance reviews while providing clinicians with comprehensive client progress visualization.
Write your best treatment plans
Ready to transform your clinical documentation?
Upheal's intelligent platform streamlines your clinical workflow while maintaining the highest standards of care. Our purpose-built features for anxiety disorder treatment help you focus on what matters most — your clients' recovery journey.
Start your free 14-day trial today and discover how intelligent documentation can enhance your clinical practice.