Stop losing money: 7 things to look for when choosing mental health billing software

If you're a mental health professional, there's a good chance you're unknowingly leaving thousands of dollars on the table every year. The culprit isn't your clinical skills or your client retention — it's your billing process.
Industry analysis suggests that behavioral health practices commonly lose anywhere from 5% to over 15% of their potential revenue to denied, underpaid, or simply forgotten claims.
That's not a rounding error; for a solo practitioner billing $150,000 annually, losing even the lower-end estimate of 5% of revenue is still $7,500 vanishing into administrative chaos.
The painful irony is that most therapists invest in billing software believing it will solve this problem, only to discover they've simply automated the easy parts while the hardest, most revenue-critical tasks remain buried and invisible.
You can submit claims all day long, but if you can't track what happens to them afterward, reconcile payments accurately, or efficiently appeal denials, you're essentially throwing darts in the dark and hoping for the best.
This article breaks down seven expert-informed considerations that separate billing software that truly protects your revenue from platforms that simply give you a false sense of security. These insights come from billing professionals who've spent years in the trenches of mental health reimbursement, and they'll help you see past the marketing promises to identify what actually matters.
Why most billing software fails therapists
The battle is won in reconciliation, not submission
Here's what most therapists don't realize until they're deep into insurance billing: submitting a claim is the easiest part of the entire process.
It's genuinely straightforward — you enter a diagnosis code, a procedure code, the date of service, and click submit. Modern software handles this beautifully, which is why nearly every platform advertises seamless claims submission as a major feature.
But submission is just the opening move.
The real battle — the place where your income is actually won or lost — happens in the weeks and months that follow.
What happens when a claim comes back denied because of a minor coding error? What about when an insurance company pays you $87 for a session when your contracted rate is $105, and there's no explanation of benefits to tell you why? Or when a claim simply disappears into the void with no response at all for 45 days?
This is where billing becomes genuinely complex work that requires detailed tracking, proactive follow-up, and strategic resubmission. You need to know the status of every single claim, apply payments correctly to client accounts, identify patterns in denials, and meet strict appeal deadlines that vary by payer.
This reconciliation work is tedious, time-consuming, and requires specialized knowledge — but it's also where 15% of your revenue is hiding.
The hidden data problem with popular EHRs
Billing experts who work across multiple platforms consistently raise one particularly frustrating complaint about many popular all-in-one electronic health record systems: they hide or overcomplicate access to the back-office data that's essential for effective reconciliation and appeals.
Think about what you need to appeal a denied claim successfully. You need the original claim data, the denial reason code, the remittance advice, any previous submission attempts, and ideally a clear aging report that shows you're approaching a filing deadline.
In platforms with poor back-office functionality, this information might be scattered across multiple screens, buried in PDFs that are difficult to search, or simply not available in an exportable format that a billing professional can actually use.
Some platforms have been described as "absurd" in their approach to financial reporting, offering only high-level summaries when what you desperately need is granular, claim-level detail.
This is beyond a mere annoyance — it's a direct threat to your revenue.
If you or your biller can't easily see which claims are aging past 30 days, you can't follow up before deadlines pass. If you can't pull a clean report of all denials from a specific payer, you can't identify whether there's a systematic issue with how you're credentialing or coding for that insurance company.
The irony is that these systems often excel at the clinical and scheduling features that therapists love, which is why they're popular. But their billing modules are frequently an afterthought, bolted on without deep consideration for the realities of revenue cycle management in behavioral health.
7 must-haves for your billing platform
1. Robust back-office reconciliation and denial management
This is the single most critical factor in choosing billing software, and it's where you should be most demanding during demos.
The platform must provide clear, intuitive, and exportable reporting that shows you the status of every single claim at a glance. You need:
- claims aging reports that automatically flag anything sitting unpaid beyond 30 days
- easy access to electronic remittance advice and denial codes
- the ability to track resubmission attempts and their outcomes.
Look for software that treats reconciliation as a first-class feature, not an afterthought.
During demos, ask to see their financial dashboard and their denial management workflow. Ask how they handle batch payment posting. Request to see an actual aging report.
If the sales representative seems confused by these questions or shows you generic financial summaries instead of claim-level detail, that's a significant red flag.
If you work with an external biller, this requirement becomes even more critical. Your biller needs seamless access to this data to do their work effectively. They shouldn't have to constantly log in, navigate through multiple screens, and manually compile information into spreadsheets just to figure out what needs attention. The platform should make their specialized expertise more powerful, not fight against it.
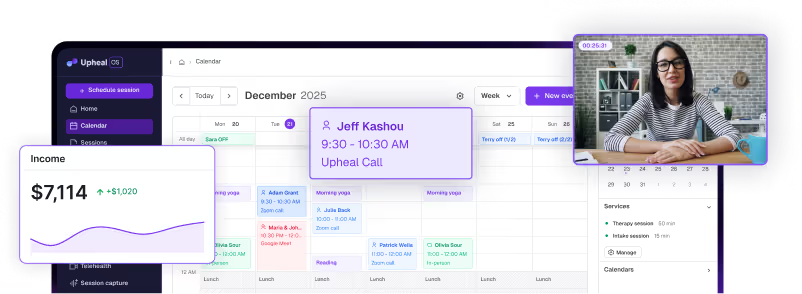
2. Seamless integration: EHR, billing, and scheduling in one place
Disconnected systems create an administrative nightmare that wastes your time and introduces countless opportunities for error.
When your clinical notes live in one platform, your schedule in another, and your billing in a third, you're forced into constant manual data transfer. That might mean physically typing appointment times from your calendar into your billing system, or even more absurdly, taking photos of your schedule to send to a biller.
The ideal system eliminates all of this friction by unifying your workflow.
When you complete a session note, the system should automatically know that the appointment happened, pull the correct procedure code based on the session length and type, and create a claim using the client's insurance information that's already stored in their chart. No separate entry. No transferring of data. No opportunity for a transcription error that results in a denied claim.
This integration also protects you from a surprisingly common source of lost revenue: forgetting to bill for sessions.
When everything is connected, you can instantly see which completed sessions haven't been billed yet. In disconnected systems, sessions can slip through the cracks for months, and by the time you realize it, the filing deadline has passed.
Think of integration not just as a convenience feature, but as a fundamental protection against both administrative burden and revenue loss. The goal is to minimize every touchpoint between your clinical work and your claims submission, because each touchpoint is a place where errors creep in and time disappears.
3. The "human-in-the-loop" oversight process
As artificial intelligence and automation become more sophisticated, there's a tempting promise in the billing world: fully automated payment posting that requires zero human intervention. A payment comes in, the system automatically applies it to the correct client account, and moves on.
This sounds efficient, but billing experts consistently warn against trusting this process completely.
The problem is that insurance payments are often messy and subtle. A claim might be partially paid with no clear explanation. A payment might arrive weeks after the session with a different date of service than expected. Two claims might be bundled together in a single payment.
In each of these scenarios, a fully automated system might misapply the payment or, worse, miss that a denial has occurred and mark the claim as resolved when money is actually still owed.
Look for a system that balances automation with oversight. The platform should automatically retrieve remittance data and suggest how to apply payments, but it should allow — or even require — a manual review step before finalizing the posting.
This human-in-the-loop approach catches the subtle denials and discrepancies that automated systems routinely miss. It's in this review process that experienced billers earn their value, spotting patterns and problems that would otherwise cost you thousands in lost revenue.
This might sound like it defeats the purpose of billing software, but it’s worth a reframe. Your software should eliminate the tedious work of gathering and organizing data, but preserve your ability to apply professional judgment to that data before making final decisions about your accounts receivable.
4. Behavioral health-specific coding and compliance
Mental health billing operates under a unique set of rules that differ substantially from medical billing.
Time-based CPT codes, the nuances of individual versus group therapy coding, the specific diagnostic requirements under DSM-5 and ICD-10 for behavioral health conditions — these are all specialized areas where generic medical billing software often falls short.
The platform you choose should have mental health coding logic built into its foundation.
It should prompt you with the correct time-based codes when you document session length.
It should help you avoid common coding errors that trigger denials, like failing to include the required number of ICD-10 codes or mismatching diagnosis codes with procedure codes in ways that raise red flags for payers.
This specialized support directly reduces your denial rate. When the software guides you toward compliant, payer-friendly coding from the start, fewer claims come back rejected for technical errors.
This is particularly valuable for therapists who are newer to insurance billing or who work with multiple payers that have slightly different requirements.
During your evaluation, ask specifically about how the platform handles behavioral health coding. Look for built-in code suggestions, validation checks, and ideally, educational resources that help you understand the reasoning behind coding decisions.
The best platforms essentially build coding expertise into the system itself, so you don't have to become an expert to bill correctly.
5. Automated front-end client management
While back-office reconciliation is where revenue is protected, front-end automation is where you save time and project professionalism to clients.
The platform should handle the initial financial steps of the client relationship automatically, removing these administrative tasks from your plate entirely.
Real-time eligibility verification is perhaps the most valuable front-end feature. Before a client's first session, the system should automatically check their insurance status through services like Availity, confirming that their coverage is active, identifying their copay amount, and flagging any issues like missing authorizations.
This prevents the awkward situation of seeing a client for weeks only to discover their insurance was never active, leaving you with a large uncollectible balance.
The platform should also securely collect, store, and process client payments automatically. When a copay or coinsurance amount is due, the system should charge the stored payment method without requiring you to manually process anything.
This improves your cash flow by ensuring prompt payment, and it creates a more professional experience for clients who appreciate not having to remember to bring payment to each session.
Look for platforms that present these features as standard capabilities, not premium add-ons. Automated eligibility checks and payment processing should be table stakes for any modern mental health billing system, and you shouldn't have to pay significantly extra for them.
6. Scalability and support for external billing professionals
Your billing needs will likely evolve as your practice grows. You might start as a solo practitioner managing everything yourself, add an external biller when the administrative work becomes overwhelming, eventually bring on associate clinicians, and possibly even transition to a group practice model.
Your software should support this entire growth trajectory without forcing you to switch platforms.
If you're considering or already using an external biller, pay close attention to how the platform handles third-party access. The system must allow you to grant secure, role-based access to your biller without giving them unnecessary access to clinical notes or other sensitive information.
The interface should be intuitive enough that an experienced biller can navigate it effectively, and it should provide the data access they need to perform proactive financial management on your behalf.
Proactive financial management means your biller can set up new client insurance information, explain benefits and payment expectations to clients, follow up on outstanding balances, and manage the entire revenue cycle without constantly needing your input.
This level of support is only possible when the software is designed with this workflow in mind.
Even if you don't currently work with a biller, choosing a platform that supports this model gives you an exit strategy when administrative work becomes unsustainable.
Therapist burnout is often driven by administrative burden, and knowing you can seamlessly add professional billing support without changing your entire tech stack is valuable optionality.
7. Reduction of clinical-to-administrative burden
This consideration underlies all the others, but it deserves explicit emphasis because it's ultimately why billing software matters.
The platform's fundamental purpose should be to minimize the time and cognitive energy you spend on administrative tasks so you can focus on what you trained for: providing excellent clinical care and thoughtfully reflecting on your clients' needs.
Therapist burnout is a genuine crisis in the mental health field, and administrative burden is a primary driver.
When you're constantly logging into systems to pull reports, manually transferring information between platforms, chasing down claim statuses, or trying to decipher cryptic denial codes, that's time and mental energy stolen from clinical work.
This isn't just about convenience or efficiency — it's about the sustainability of your practice and your career.
Evaluate every platform feature through this lens.
Does this feature genuinely reduce your administrative workload, or does it simply give the appearance of sophistication while still requiring substantial manual intervention?
If you find yourself spending significant time gathering data, reconciling accounts, or figuring out what needs attention, the software has failed its core mission regardless of how many other features it offers.
The best billing platforms feel almost invisible in your daily workflow. They handle the complexity in the background, surface only the information that requires your decision or action, and protect your revenue without demanding constant attention.
This is what you should expect, and what you should demand when evaluating options.
Using a platform yourself vs. outsourcing
Understanding the seven must-haves helps clarify which billing model makes sense for your practice, because each model represents different trade-offs between cost, control, and expertise. Let's examine the two primary approaches and what they mean for your practice.
🎁 The all-in-one platform approach
Systems like SimplePractice or TherapyNotes let you handle everything yourself, offering significant advantages.
These platforms are typically cost-effective with predictable monthly fees, and they streamline your front-office operations beautifully by integrating notes, scheduling, and billing in one place. For newer practices or those with primarily self-pay clients, this model can work well.
However, the limitation is that these platforms often lack the back-office functionality and specialized expertise necessary to maximize insurance reimbursement. You're responsible for learning insurance billing yourself, staying current on coding changes, and managing the reconciliation and appeals process.
This can be overwhelming, particularly when combined with the demands of clinical work. If the platform doesn't excel at providing the robust back-office tools described in consideration one, you may find yourself losing revenue to denied claims that never get appealed or underpayments that never get questioned.
💸 The outsourced or professional biller model
This approach flips the equation entirely. You typically pay a percentage of collections — commonly 5-8% — but in exchange, you gain access to specialized billing expertise.
Experienced billers know the nuances of different payers, can navigate complex denial scenarios, and often achieve higher overall reimbursement rates through effective appeals and proactive follow-up. You also free yourself from the administrative burden entirely, which can be transformative for preventing burnout.
The trade-off is cost and some loss of direct control. You're paying more, and you're trusting someone else to manage a critical part of your revenue cycle.
This model works best when combined with software that supports external biller access — consideration six from our list. You need a platform that makes it easy for your biller to do excellent work on your behalf without creating friction or limiting their effectiveness.
There's no universally correct choice here. The right model depends on your practice size, your comfort with administrative work, your payer mix, and your priorities around time versus money. The key is to make an informed choice while understanding that the seven considerations apply regardless of which path you choose.
Choosing what’s right for your practice
Our core guidance here is simple but important: prioritize robust back-end features over flashy front-end automation.
Yes, automated appointment reminders and digital intake forms are nice conveniences, but they don't protect your revenue.
What protects your revenue is clear financial reporting, effective denial management, and systems that support thorough reconciliation.
When evaluating platforms, request demos that focus specifically on the billing and financial management features, not just the clinical and scheduling tools.
Here's what to ask for during your evaluation:
- show me your aging reports
- walk me through your denial tracking workflows
- show how payment application works in your system
- demo typical complex scenarios, like a partial payment with an unclear denial reason
If the sales team struggles to demonstrate these capabilities or dismisses them as unimportant, that's valuable information.
Take advantage of free trials, but use them strategically. Don't just test whether you can create notes and schedule appointments — everyone does that well. Instead, test the billing workflow end-to-end.
Submit some test claims, see how payments are applied, check what reports are available. Imagine yourself three months into using the system, trying to figure out why you're still owed money on a claim from sixty days ago, and ask yourself whether this platform gives you the tools to solve that problem efficiently.
The right billing software should feel like hiring a highly competent financial manager who handles complexity in the background and gives you clear, actionable information when you need it.
It should reduce your administrative burden genuinely, not just reorganize it.
And most importantly, it should protect the revenue you've rightfully earned by providing the tools necessary to track, reconcile, and fight for every dollar that insurance companies owe you.
Your practice deserves software that works as hard as you do. Choose accordingly.








.avif)

![Best scheduling software for therapists [2026]](https://cdn.prod.website-files.com/6328c07d72b05347cc236c49/68dd9ec24d044bac7d15aa1a_Best%20scheduling%20software%20thumbnail.avif)