A clinician’s guide to therapy scheduling

A clinician's guide to therapy scheduling
You've mastered therapeutic interventions and built genuine connections with clients.
Now you're staring at an empty calendar, wondering how to manage the business side of your practice.
Scheduling overwhelms many clinicians because graduate programs focus on clinical training, not appointment logistics.
Most independent therapists develop these systems through trial and error.
Clinical expertise meets business reality
Your graduate program prepared you to heal, not to manage appointments. Clinical training covers trauma-informed care and therapeutic alliance. Calendar management? Cancellation policies? Crisis protocols? These skills develop through practice experience.
This creates anxiety for many new practitioners. You might feel uncertain during those early months, gathering advice from colleagues or online forums to build your administrative approach.
The learning curve is real, but thousands of therapists have navigated this transition successfully. Your clinical skills translate into business wisdom more directly than you might expect.
Your schedule shapes how effective you are
Your scheduling approach directly impacts both your wellbeing and your therapeutic work.
Consider your energy patterns throughout the week. Maybe you're sharpest during morning sessions but struggle with focus after 3pm. Perhaps back-to-back appointments drain you, or you prefer intensive session blocks with longer breaks between clients.
These preferences aren't just personal comfort — they're clinical considerations. Burnout compromises therapeutic effectiveness.
Your scheduling choices also model healthy boundaries for clients. When you protect your time and energy consistently, you demonstrate the self-respect and work-life balance you encourage them to develop.
Manual versus automated scheduling
Most therapists face this fundamental choice: manage appointments personally or use automated booking systems.
Manual scheduling advantages:
You handle every booking personally, which allows:
- Client screening during initial contact
- Direct control over practice composition
- Personal touch that builds rapport
- Protection from technical system failures
Manual scheduling requires constant phone coordination, creates scheduling conflicts, and consumes clinical time for administrative tasks.
Automated system benefits:
Modern booking platforms handle scheduling automatically:
- 24/7 client booking availability (often when people search for help)
- Eliminated phone tag and communication delays
- Reduced double-booking and human error
- Protected clinical time for therapeutic work
Many therapists worry about losing practice control with automated systems.
Current scheduling platforms include professional safeguards. You can limit new client session quantities, prevent same-day appointments, or block specific time slots. Technology has evolved to address therapists' boundary maintenance concerns.
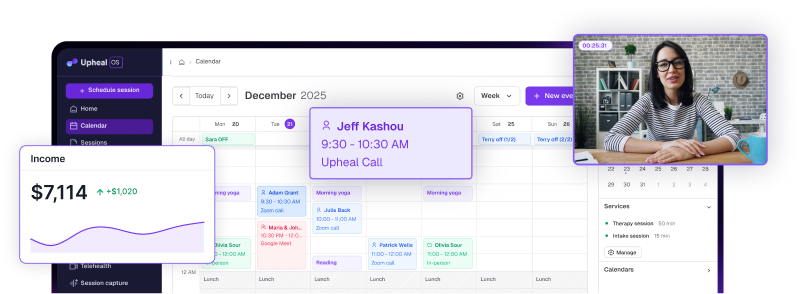
Selecting practice management software
Your Electronic Health Record (EHR) becomes your practice backbone. It manages scheduling, billing, notes, and client communication through integrated systems.
Solo practitioners especially benefit from unified platforms that prevent multi-system coordination chaos.
Essential EHR requirements
Non-negotiable features:
- HIPAA compliance verification
- Reliable customer support access
- Integrated telehealth capabilities
- Streamlined billing processes
Quality-of-life enhancements:
- Client self-service portal
- Automated appointment reminders
- Mobile platform access
- Customizable note templates
Clinician-informed platform comparison
Cancellation policy considerations
The standard 24-hour cancellation rule generates significant debate among therapists. This policy often produces counterproductive results.
Most therapists don't maintain waitlists of people ready to fill last-minute appointment slots. Twenty-four-hour notice doesn't actually protect income in these situations.
The policy encourages clients to cancel early "just in case" rather than attending when they actually could participate. This increases cancellations rather than reducing them.
Many therapists experience guilt enforcing cancellation fees. Clinical training emphasizes understanding and support — charging someone for migraines or childcare emergencies feels professionally inconsistent.
Consider reframing: clear cancellation policies model healthy boundaries. They demonstrate that professional time holds value and commitments carry meaning.
Alternative policy approaches:
⚾ Three-strike system: Allow several free cancellations before implementing fees. This provides grace while maintaining professional limits.
🔜 Same-week reschedule option: Waive fees when clients reschedule within the current week. This encourages rebooking rather than simple cancellation.
💸 Financial circumstance considerations: Adjust policies based on client economic situations when clinically appropriate.
Communicate policies clearly during intake, then enforce consistently. Inconsistent enforcement creates confusion and resentment for both parties.
Ethical waitlist management
Full practices create positive challenges: managing people who want services but can't access immediate appointments.
Always conduct brief phone screenings to assess crisis situations before waitlist placement.
Effective waitlist practices:
✋ Realistic expectation setting: Communicate honest wait times. "I typically have openings in 6-8 weeks" helps people make informed decisions about their care.
📞 Resource provision: Offer referrals to other therapists, crisis hotlines, or self-help resources for interim support rather than requesting passive waiting.
📨 Consistent communication: Check in periodically with waitlisted clients. Brief emails every few weeks demonstrate ongoing professional attention.
💻 Technology integration: Manual spreadsheet tracking creates missed opportunities and client frustration. EHR systems automate much of this coordination process.
Some therapists worry that waitlist maintenance creates false security — people often locate other therapists rather than waiting. This is professionally appropriate. Your responsibility involves providing options and support, not guaranteeing future availability.
Crisis management boundaries
You are not a crisis hotline. This boundary protects both your professional sustainability and client safety.
Your ethical obligation ensures clients know how to access help when you're unavailable. This occurs through collaborative crisis planning, not continuous availability.
Crisis plan components:
🫂 Support network identification: Who can clients contact when struggling? List trusted friends, family members, or other supports in priority order.
🕟 Professional availability: Clearly state business hours and communication protocols for during and after-hours contact.
⚠️ Personal warning signs: Help clients identify individual early crisis indicators. This might include sleep pattern changes, increased isolation, or specific thought patterns.
📋 Coping strategy menu: Develop personalized healthy coping skills clients can use independently. Include immediate strategies (deep breathing, walking) and longer-term approaches (exercise routines, creative outlets).
☎️ Professional crisis resources: Provide specific crisis hotlines, emergency room information, and after-hours mental health services in your geographical area.
Crisis planning evolves as you learn individual client patterns and needs through ongoing therapeutic work.
If you spend significant time managing crisis situations outside regular sessions, billing for that time is professionally appropriate. Ensure your informed consent clearly explains this policy.
Sustainable schedule development
Your optimal schedule balances personal energy, client needs, and financial sustainability.
☕ Energy pattern recognition: Schedule challenging clients during your peak performance periods. If you're most alert mornings, avoid placing difficult sessions late in the day.
☀️ Client preference accommodation: Some people require evening appointments due to work schedules. Others prefer morning sessions. Building options helps serve diverse populations.
🏃 Long-term sustainability planning: A schedule that works short-term but creates burnout isn't actually functional. Consider what you can maintain over years of practice.
Practical scheduling approaches:
‼️ Session clustering: Some therapists prefer appointment blocks (five consecutive sessions) to minimize transition time and maximize focus.
🍵 Distributed scheduling: Others perform better with client breaks for decompression and session preparation.
👩💻 Administrative time blocking: Schedule specific hours for notes, treatment planning, and business tasks. Avoid squeezing administrative work into inadequate time gaps.
⌛ Schedule buffer integration: Consider padding your calendar to accommodate sessions that extend beyond scheduled time or unexpected clinical needs.
Technology as clinical support
Modern scheduling platforms function as intelligent practice partners that adapt to your professional workflow rather than requiring workflow adaptation to technology.
Advanced features for consideration:
- Automated reminder systems that measurably reduce no-show rates
- Booking parameters that maintain professional boundaries automatically
- Integrated billing that streamlines financial processes
- Practice analytics that reveal schedule optimization opportunities
When scheduling technology integrates seamlessly with clinical workflow, you create more space for therapeutic presence with clients.
Effective scheduling supports sustainable clinical practice rather than perfect appointment management. Your clinical expertise includes the professional judgment needed for practice management. Learn from colleague experiences while trusting your clinical instincts about what works for your specific practice and client population.
Administrative systems that function smoothly in the background allow complete focus on the therapeutic relationships that make clinical work meaningful.