ICD-10 code for alcohol dependence with intoxication, delirium

F10.221 is the ICD-10 code for alcohol dependence with intoxication, delirium.
This diagnostic code represents a serious medical emergency where someone with alcohol dependence experiences both acute intoxication and delirium tremens (DTs).
Accurate diagnosis and prompt treatment are critical, as alcohol withdrawal delirium carries significant morbidity and a historical mortality rate as high as 15%, though modern management has reduced this to less than 1%.
Key features:
- F10.221 captures the intersection of three clinical presentations: established alcohol dependence syndrome, current alcohol intoxication, and acute delirium requiring immediate medical intervention
- Delirium typically emerges two to three days after drinking cessation or reduction, though it can occur while blood alcohol levels remain elevated in severe dependence
- This diagnosis requires hospitalization with close monitoring, benzodiazepine loading protocols, and management of concurrent medical complications like dehydration, electrolyte imbalances, and thiamine deficiency
- Proper documentation improves continuity of care and supports appropriate treatment intensity for this life-threatening complication of alcohol dependence
Diagnostic criteria for alcohol dependence with intoxication, delirium (F10.221)
Clinicians assign F10.221 when three distinct clinical elements converge in the same patient presentation.
First, the individual meets criteria for alcohol dependence, which requires at least two symptoms from a constellation that includes impaired control over drinking, alcohol use becoming an increasing priority despite negative consequences, and physiological features like tolerance or withdrawal.
The dependence component indicates a pattern of repeated alcohol use where the substance takes precedence over other life activities.
Second, the patient presents with current alcohol intoxication at the time of evaluation. This means detectable blood alcohol levels or recent consumption causing behavioral, psychological, or physiological changes.
Third, and most critically, the patient exhibits delirium. The delirium component includes:
- Disturbance in attention—reduced ability to direct, focus, sustain, and shift attention—combined with reduced awareness of the environment
- Acute onset developing over hours to days, representing a change from baseline that fluctuates throughout the day
- Additional cognitive disturbances such as memory deficits, disorientation, language problems, visuospatial difficulties, or perceptual disturbances
- Evidence from history, physical examination, or laboratory findings that the disturbance results directly from alcohol intoxication or withdrawal
- Symptoms not better explained by another neurocognitive disorder or severely reduced arousal like coma
Accompanying features often include autonomic hyperactivity with elevated temperature, rapid heart rate, high blood pressure, and profuse sweating. Patients may experience visual, tactile, or auditory hallucinations alongside paranoid thinking and severe agitation.
When to use F10.221 diagnosis code
Understanding when F10.221 applies versus related codes ensures accurate diagnosis and appropriate treatment.
The key differentiating factor for F10.221 is the presence of delirium during intoxication in someone with established alcohol dependence. Without delirium, different codes apply.
F10.221 vs F10.220 (alcohol dependence with intoxication, uncomplicated)
F10.220 describes alcohol dependence with current intoxication but without delirium or other complications. Use this code when the patient shows signs of intoxication—slurred speech, impaired coordination, behavioral changes—but maintains normal consciousness and orientation.
Choose F10.221 when confusion, disorientation, or altered consciousness accompanies the intoxication. The distinction matters because F10.220 typically requires supportive care and monitoring, while F10.221 demands immediate intensive intervention.
F10.221 vs F10.22 (alcohol dependence with intoxication)
F10.22 serves as the parent code for alcohol dependence with intoxication. The fourth digit specifies whether complications exist.
F10.221 includes that fourth digit to indicate delirium specifically. This specificity guides treatment teams toward protocols for managing this life-threatening emergency rather than standard intoxication care.
F10.221 vs F10.231 (alcohol dependence with withdrawal, delirium)
This comparison presents a common clinical challenge. Both codes involve delirium in someone with alcohol dependence, but the timing and presence of intoxication differ.
Use F10.231 when delirium occurs during withdrawal after alcohol cessation, typically without current intoxication. Blood alcohol levels are low or zero, and symptoms emerge as alcohol clears from the system.
Choose F10.221 when delirium manifests while the patient remains intoxicated. This scenario can occur in severe dependence where withdrawal symptoms begin even with elevated blood alcohol levels, or when delirium develops before intoxication fully resolves.
The distinction affects immediate management. F10.231 requires aggressive benzodiazepine loading to suppress withdrawal, while F10.221 may need additional consideration of persistent intoxication effects alongside emerging withdrawal.
Related ICD-10 codes
Clinicians should be aware of these related codes within the F10.2 family:
- F10.20 - Alcohol dependence, uncomplicated
- F10.22 - Alcohol dependence with intoxication (parent code)
- F10.220 - Alcohol dependence with intoxication, uncomplicated
- F10.229 - Alcohol dependence with intoxication, unspecified
- F10.23 - Alcohol dependence with withdrawal
- F10.230 - Alcohol dependence with withdrawal, uncomplicated
- F10.231 - Alcohol dependence with withdrawal, delirium
- F10.232 - Alcohol dependence with withdrawal with perceptual disturbance
- F10.239 - Alcohol dependence with withdrawal, unspecified
- F10.24 - Alcohol dependence with alcohol-induced mood disorder
- F10.25 - Alcohol dependence with alcohol-induced psychotic disorder
Interventions and CPT codes for alcohol dependence with intoxication, delirium
Treatment for F10.221 involves acute medical stabilization followed by comprehensive substance use treatment.
Emergency medical management
The immediate priority involves controlling agitation and preventing medical complications. Patients require hospitalization with continuous monitoring of vital signs, hydration status, and consciousness levels.
Medical management includes rapid benzodiazepine loading—typically diazepam 10-20 mg orally every one to two hours until reaching 60-80 mg total or achieving light sedation. Doses may need to exceed 120 mg with specialist consultation. This aggressive approach reduces mortality and delirium duration.
Clinicians also administer parenteral thiamine at least 500 mg two to three times daily to prevent Wernicke encephalopathy. Intravenous fluids correct dehydration and electrolyte abnormalities, particularly magnesium deficiency.
When adequate benzodiazepine doses fail to control agitation, antipsychotic medications like haloperidol 2.5-10 mg, olanzapine 5-10 mg, or risperidone 1-5 mg provide additional symptom relief. Antipsychotics should never replace benzodiazepines, only supplement them.
Environmental modifications help reduce disorientation. A quiet room with minimal stimulation, good lighting, and clear environmental cues like clocks and calendars supports recovery. One-to-one supervision may be necessary for safety.
Relevant CPT code: 90791 - Psychiatric diagnostic evaluation (for comprehensive initial assessment once medically stabilized)
Cognitive behavioral therapy
Once acute delirium resolves, evidence-based psychotherapy addresses underlying alcohol dependence. Cognitive behavioral therapy (CBT) stands as the gold standard psychosocial intervention.
CBT for alcohol dependence typically involves 12 weekly individual sessions. Treatment helps patients identify and modify dysfunctional thinking patterns about alcohol, recognize high-risk situations, develop effective coping strategies, and increase non-drinking activities.
Specific CBT components include coping skills training, relapse prevention strategies, cognitive restructuring around alcohol expectancies, and problem-solving techniques. Modern practice combines CBT with motivational interviewing during initial sessions to resolve ambivalence about change.
Relevant CPT codes:
- 90832 - Psychotherapy, 30 minutes (16-37 minutes)
- 90834 - Psychotherapy, 45 minutes (38-52 minutes)
- 90837 - Psychotherapy, 60 minutes (53+ minutes)
Choose the code matching actual session duration. Documentation should include specific CBT techniques used and treatment goals addressed.
Motivational interviewing
For patients ambivalent about abstinence or change, motivational interviewing helps explore and resolve this uncertainty. This counseling style guides individuals toward recognizing discrepancies between current drinking and broader life goals.
Motivational interviewing works particularly well as a standalone brief intervention for less severe dependence or as preparation before more intensive treatment. The approach emphasizes collaboration, evokes the patient's own reasons for change, and respects autonomy rather than imposing change.
Core strategies include expressing empathy through reflective listening, developing discrepancy between current behavior and values, managing resistance without argument, and supporting self-efficacy for change.
Relevant CPT codes:
- 99408 - Alcohol screening with brief intervention, 15-30 minutes (commercial insurance)
- 99409 - Alcohol screening with brief intervention, greater than 30 minutes (commercial insurance)
- G0396 - Alcohol structured assessment with brief intervention, 15-30 minutes (Medicare)
- G0397 - Alcohol structured assessment with brief intervention, greater than 30 minutes (Medicare)
Document the screening tool used (such as AUDIT or AUDIT-C), score obtained, risk level identified, and specific brief intervention elements provided.
Family therapy
Alcohol dependence affects entire family systems. Family therapy addresses relationship dynamics, codependency patterns, and develops family-based relapse prevention plans.
Working with family members provides collateral information about drinking patterns, helps identify environmental triggers, and builds a support network for recovery. Family involvement often improves long-term outcomes.
Relevant CPT codes:
- 90846 - Family psychotherapy without patient present
- 90847 - Family psychotherapy with patient present
Group therapy
Many patients benefit from group-based substance use treatment. Group therapy provides peer support, reduces isolation, allows practicing skills in a social context, and normalizes recovery experiences.
Common group formats include process groups focusing on interpersonal dynamics, skills-based groups teaching specific coping techniques, and relapse prevention groups addressing high-risk situations.
Relevant CPT code: 90853 - Group psychotherapy
Pharmacotherapy for relapse prevention
Once withdrawal resolves and the patient achieves initial stabilization, medications support long-term abstinence. Three medications have strong evidence for alcohol dependence: naltrexone, acamprosate, and disulfiram.
Naltrexone blocks opioid receptors, reducing alcohol's rewarding effects and decreasing craving. Acamprosate modulates glutamate neurotransmission, helping restore neurochemical balance disrupted by chronic alcohol use.
Disulfiram produces unpleasant reactions when combined with alcohol, creating a deterrent.
Pharmacotherapy works best when combined with psychotherapy rather than used alone. The choice among medications depends on patient preferences, medical history, and treatment goals.
Relevant CPT code: 90863 - Pharmacologic management (when provided during psychotherapy visit)
Crisis intervention
Patients in acute distress related to their alcohol dependence may require crisis psychotherapy. This might involve managing suicidal ideation, addressing acute consequences of drinking, or intervening during periods of high relapse risk.
Relevant CPT codes:
- 90839 - Psychotherapy for crisis, first 60 minutes
- 90840 - Psychotherapy for crisis, each additional 30 minutes (add-on code)
Document the crisis nature of the presentation, imminent risk factors, and crisis intervention strategies employed.
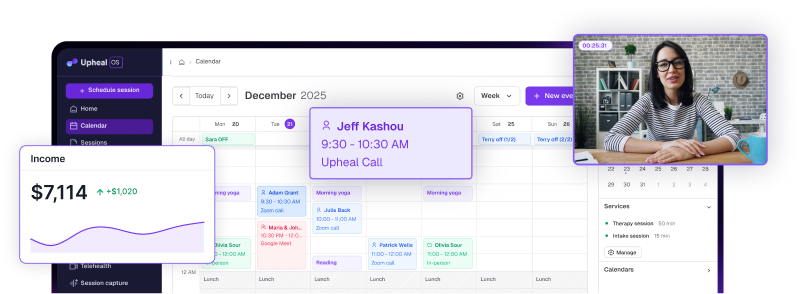
How Upheal improves F10.221 ICD-10 documentation
Clinical documentation platforms help therapists manage the complex requirements of treating alcohol dependence with delirium.
Suggesting appropriate ICD-10 codes based on session content
Upheal's clinical documentation platform analyzes session notes and conversation patterns to identify relevant diagnostic indicators. When session content discusses delirium symptoms during intoxication in a patient with established alcohol dependence, the platform can suggest F10.221 as the appropriate code.
This assistance proves valuable because F10.221 requires recognizing three simultaneous clinical features — dependence, intoxication, and delirium. The platform helps clinicians capture this specificity rather than defaulting to less precise codes.
The code suggestion feature draws from session documentation about confusion, disorientation, fluctuating consciousness, and timeline of symptom onset. This supports accurate diagnosis even in complex presentations where multiple substance-related issues overlap.
Maintaining HIPAA-compliant records with proper diagnostic coding
Proper diagnostic coding serves multiple purposes beyond billing. Accurate F10.221 documentation creates a medical record that supports care coordination when patients transition between emergency departments, inpatient units, and outpatient follow-up.
Upheal maintains HIPAA-compliant storage of all clinical documentation. The platform's security infrastructure protects sensitive information about substance use, delirium episodes, and treatment history while ensuring records remain accessible to authorized providers.
For F10.221 cases, this documentation continuity matters significantly. Future providers need clear records of delirium episodes to assess seizure risk, gauge withdrawal severity, and make informed decisions about treatment intensity.
Reducing administrative burden so you can focus on client care
Patients recovering from alcohol withdrawal delirium need intensive clinical attention. They face elevated risk of relapse, often have co-occurring medical complications, and require careful monitoring during early recovery.
Upheal's automated documentation features handle time-consuming administrative tasks like generating progress notes, organizing session content, and maintaining treatment timelines. This automation frees clinicians to concentrate on therapeutic work rather than paperwork.
The platform can generate structured progress notes that capture essential elements for F10.221 cases: current mental status, substance use patterns, withdrawal symptom severity, treatment response, and relapse risk factors. These comprehensive notes support continuity of care while requiring minimal clinician time.
For busy therapists managing multiple complex cases, reducing documentation time by even 15-20 minutes per session creates meaningful capacity for additional clinical work or self-care.
Supporting clients with alcohol dependence, intoxication, and delirium
Patients diagnosed with F10.221 have survived a life-threatening medical emergency. The path forward requires addressing both immediate stabilization and long-term recovery needs.
Recovery from alcohol dependence with delirium starts with recognition that this diagnosis indicates severe substance use requiring intensive intervention.
Brief encounters with primary care or emergency departments rarely suffice.
These patients benefit from specialized addiction treatment, often beginning with residential rehabilitation following medical stabilization.
The delirium episode itself may have caused significant fear and confusion for both patient and family.
Providing psychoeducation about what occurred, why delirium developed, and how to prevent recurrence helps reduce anxiety and improves treatment engagement.
Patients often don't remember their delirium clearly, so filling in these gaps with compassionate explanation supports psychological processing.
Long-term treatment plans must address underlying factors that led to severe dependence: trauma history, co-occurring mental health conditions, social isolation, chronic stress, or other substance use.
Comprehensive assessment guides treatment matching to appropriate intensity and modality. Some patients need residential programs offering 24-hour support, while others succeed in intensive outpatient programs paired with mutual support groups.
For therapists working with these clients in outpatient settings, maintaining realistic expectations helps. Alcohol dependence severe enough to cause delirium represents years of problematic use. Recovery unfolds gradually, with setbacks common.
Celebrating small victories—attending appointments consistently, one week of abstinence, reconnecting with family—builds momentum toward lasting change.
Clinical documentation platforms like Upheal support this long-term work by maintaining comprehensive treatment records, tracking progress over time, and suggesting appropriate codes as clinical presentations evolve.
Whether patients maintain abstinence, experience relapse requiring F10.221 recoding, or progress to uncomplicated remission codes, accurate documentation tells their recovery story.
Start improving your clinical documentation and spend more time with clients rather than paperwork. Try Upheal free and see how AI-assisted notes can support your practice in treating complex conditions like alcohol dependence with delirium.