Software companies still don’t get scheduling for therapists
There's a moment that happens in therapy practices across the country, usually around 8:47 AM on a Tuesday.
A client cancels last-minute, and suddenly you're juggling your personal calendar, your EHR, and the directory the client used to find you.
You’re canceling the session in three different places to make sure an insurance claim won’t be created, double-checking your client won’t be billed for a no-show, and also making sure you remember where you left things off with the client you’re seeing in five minutes — actually, now it’s four minutes.
Moments like these make it clear: the people who built your practice management software have never sat across from someone having a panic attack.
After talking to hundreds of therapists about their daily workflow struggles, one thing becomes clear: software companies are building scheduling tools for a version of healthcare that doesn't exist in therapy offices.
Scheduling for therapy is different
Most scheduling software treats appointments like they're interchangeable blocks of time. Book a slot, show up, complete transaction, next.
But therapy doesn't work that way.
When Marcus books his first appointment after three months of considering therapy, he's not scheduling a teeth cleaning. He's taking a terrifying step toward vulnerability.
When Sarah needs to cancel because her depression flared up, that's not a "no-show" to punish with policy reminders — it's clinical information that matters for her care.
Yet most practice management systems approach therapy scheduling like it's a dentist's office. Same reminder templates, same cancellation policies, same assumption that "efficiency" means squeezing more appointments into less time.
The result? Software that actively works against therapeutic relationships instead of supporting them.
The insurance nightmare nobody talks about
Here's what software developers apparently don't know: behavioral health insurance verification takes three times longer than medical insurance verification.
The average therapist spends 24 minutes per client confirming coverage, navigating prior authorization requirements, and deciphering whether session #8 or session #12 is when benefits expire.
Most of this happens after the client is already scheduled, creating a cascade of unpaid administrative work.
At the same time, EHR companies proudly demo features like "automated eligibility checks" that work beautifully for primary care but fail spectacularly when faced with the labyrinth of mental health coverage limitations.
We're not asking for miracles here. We're asking for software that understands that "covered" doesn't mean the same thing in therapy as it does in family medicine.
The illusion of integration
The promise is always the same. One login, one system, one seamless workflow. Your one-stop shop for practice management!"
The reality is different. Even the most expensive, "fully integrated" therapy EHRs still require therapists to:
- Manually verify insurance after automated checks fail
- Call clients to discuss cash pay when coverage gaps emerge
- Export data manually where bulk operations don't exist
- Correcting automated CPT codes to avoid getting flagged for an audit
“Want to change session statuses, supervisor assignments, or correct billing details across many sessions? Too bad — you have to do it one-by-one. This limitation has cost us well over 30 hours just trying to clean up old sessions.”
Dr. Elka Jacobs-Pinson on TherapyNotes
Integration isn't just about having all your tools in one platform. It's about understanding how clinical work actually flows from scheduling through documentation through billing.
Most EHRs integrate the wrong things while leaving therapists to manually bridge the gaps that actually matter.
The human element software ignores
“I really hate using my computer in sessions. I have to get up from my chair and go check it for scheduling at the end of each session. It's exhausting. But really, I would prefer to have something next to my chair where I'm talking to folks. It feels like an interruption.”
via Reddit
Therapy scheduling isn't just logistics — it's often the first point of clinical contact.
The way someone books their first appointment, how they handle cancellations during mental health crises, whether they can easily reschedule when life falls apart — these interactions set the tone for therapeutic work.
But scheduling software treats these moments like data entry problems to solve rather than relationship opportunities to support.
When someone calls to cancel because they're having the worst day of their life, they shouldn't have to navigate phone trees or complicated online forms. There’s a reason behavioral health practices typically see missed appointments at a rate of 20-30%.
When a client needs urgent support, booking shouldn't require filling out 15 intake fields.
Good scheduling software for therapists would recognize that the person booking might be in crisis, that cancellations often carry clinical meaning, that flexibility isn't a "nice-to-have" — it's essential for this kind of work.
The missed opportunity
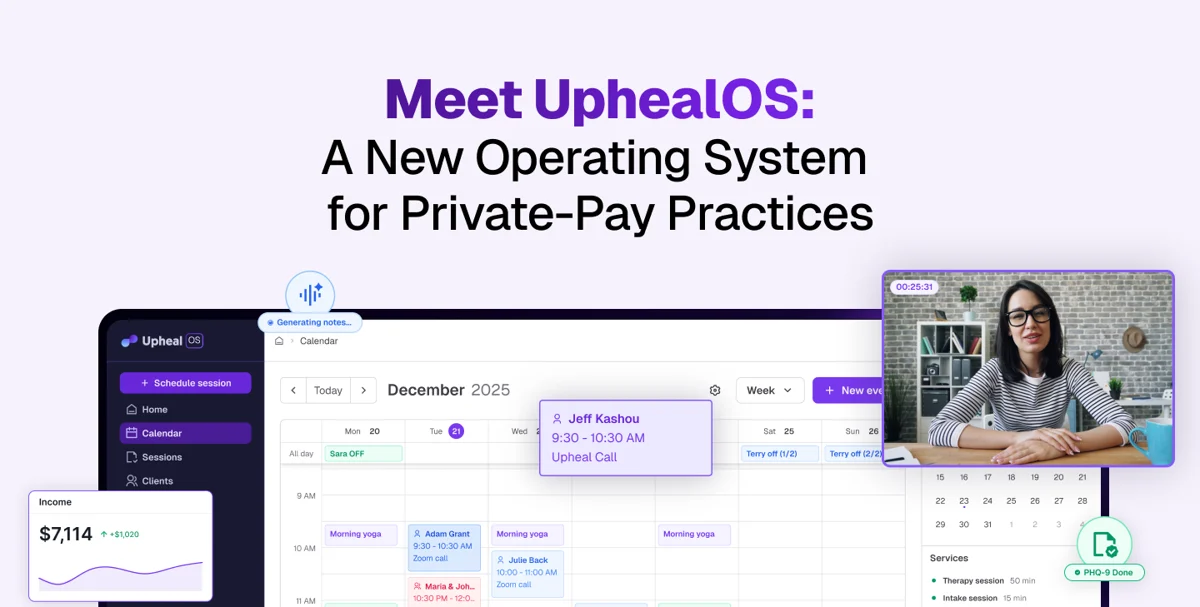
Here's what's frustrating: the technology exists to do this better.
We have AI that can detect emotional distress in text messages. We have systems that can predict no-shows based on behavioral patterns. We have integration capabilities that could seamlessly connect proactive insurance verification with scheduling with treatment planning.
But instead of applying these technologies to the genuine complexities of behavioral healthcare, most software companies just port over features that work for medical practices and call it specialized.
The result is software that technically functions but fundamentally misunderstands the work.
What actual understanding would look like
Scheduling software built by people who understand therapy would:
💓 Recognize emotional context
Booking interfaces designed for people who might be in crisis. Cancellation policies that account for mental health realities. Communication that feels supportive, not transactional.
✔️ Handle insurance complexity proactively
Real-time coverage verification that understands behavioral health benefits. Automatic conversion to cash pay when insurance fails. Clear communication about costs before appointments happen.
🛡️ Support therapeutic boundaries
Built-in buffer time between emotionally intensive sessions. Protection against back-to-back trauma appointments. Scheduling that preserves therapist wellbeing as a clinical necessity.
🪡 Integrate around clinical workflow
Systems that connect scheduling to treatment planning to outcome tracking — not just billing to documentation to compliance reporting.
The path forward
The irony is that therapists are often early adopters of technology that actually works.
We embraced telehealth before the pandemic made it mainstream. We use apps for therapy homework, digital tools for outcome tracking, online platforms for professional development.
We're not opposed to innovation. We're opposed to solutions that create more problems than they solve.
Software companies that want to serve behavioral healthcare need to spend time in therapy offices, not just with practice owners making purchasing decisions.
They need to understand that "efficiency" in therapy looks different than efficiency in primary care.
They need to recognize that good scheduling software for therapists isn't just about calendar management — it's about supporting the essential human work of healing.
Until that happens, therapists will continue to jury-rig solutions that work around software instead of with it.
We'll keep spending 20% of our time on administrative tasks that should take 5%.
We'll keep choosing between systems that are expensive but inadequate, or affordable but impossible to use.
The technology to do better exists. The understanding of what "better" means in behavioral healthcare is what's missing.
And that gap — between what's technically possible and what's clinically useful — is costing more than money. It's costing therapist energy that belongs with clients, and client experiences that should feel supportive instead of bureaucratic.
It’s time to level up software for therapists.