Checkpoint EHR gets AI that actually understands therapy

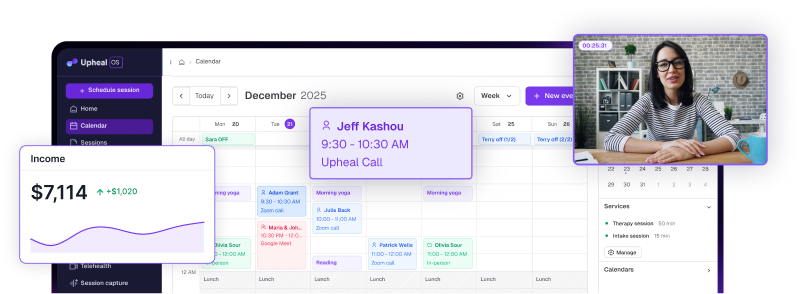
Checkpoint EHR users now have access to Upheal's AI-assisted progress notes directly within their existing workflow.
You know the documentation challenge. Session ends with meaningful therapeutic progress, client demonstrates genuine insight, and now you need to translate that clinical moment into structured documentation.
This challenge becomes even more pressing for practices facing strict payer deadlines and compliance requirements.
The Checkpoint-Upheal integration addresses this workflow interruption through intelligent documentation support built into your familiar EHR interface.
AI progress notes within Checkpoint
Here's what actually happens during session documentation with the integration. You're implementing exposure therapy with a client experiencing agoraphobia. The session includes hierarchy development, in-vivo practice planning, and anxiety rating discussions.
Upheal captures session audio in the background while you maintain therapeutic focus. After the client leaves, you click "Enhance with AI" within your Checkpoint progress note section.
Generated documentation appears formatted in your preferred template:
The AI identified your specific therapeutic intervention, documented measurable outcomes, and captured treatment planning elements using appropriate clinical language.
What the AI recognizes in therapy sessions
The technology recognizes different therapeutic modalities and documents them accordingly within Checkpoint. CBT interventions get formatted differently than psychodynamic interpretations. EMDR sessions include target memory processing and resource installation documentation. DBT skills training gets documented with specific module references and homework assignments.
Safety concerns get highlighted automatically within Checkpoint. Suicidal ideation, substance use patterns, trauma disclosures appear flagged for clinical attention rather than buried in regular text.
The system learns your documentation style over multiple sessions, picking up your preferred clinical language and theoretical frameworks.
This comprehensive documentation approach helps practices meet regulatory compliance standards and withstand audit scrutiny.
How it works within your existing Checkpoint system
The partnership eliminates switching between platforms and transferring data. Everything happens within your established EHR using familiar navigation and the same security you already trust.
Notes appear right away
Generated notes show up in Checkpoint immediately after sessions end. No waiting for processing, separate logins, or workflow interruption. You can review and edit using Checkpoint's standard tools or come back later knowing the foundation is already there.
This immediate availability is crucial for practices needing to meet strict payer deadlines for signed notes, often within 24-48 hours.
Works with your note templates
The integration supports multiple progress note formats within Checkpoint's template system. SOAP, BIRP, DAP, GIRP formatting adapts to your practice requirements and theoretical orientation while keeping documentation quality consistent.
Real practice examples
Solo practice time savings
A private practitioner seeing 20 weekly clients typically spends 5-6 hours on progress note completion. With AI assistance, documentation time drops to 90 minutes weekly — mostly review and minor editing within Checkpoint.
Group practice consistency
Administrative oversight gets simpler when all clinicians use consistent AI-assisted documentation within Checkpoint. Note quality becomes standardized across providers while preserving individual clinical voices.
Community mental health and Medicaid compliance
Practices accepting Medicaid face particularly strict documentation requirements with tight deadlines. In North Carolina, for example, Medicaid requires notes to be finalized and signed within 24 hours, with "late notes" submitted within 7 days. AI-assisted documentation helps these practices meet these critical timelines consistently.
Beyond speed, comprehensive AI-generated notes protect against audit risks that could result in payment clawbacks. When every session includes detailed intervention descriptions, risk assessments, and proper clinical formatting, practices can confidently submit claims knowing their documentation will withstand scrutiny. For community mental health centers operating on thin margins, this audit protection and faster billing turnaround can be the difference between financial stability and constant cash flow stress.
You stay in control
The technology generates draft content within Checkpoint. You review, modify, and approve all documentation before it becomes permanent. Clinical responsibility stays with licensed professionals.
Critical information gets highlighted within Checkpoint. Safety concerns, medication mentions, diagnostic considerations appear flagged for your attention.
This systematic flagging helps ensure compliance with documentation requirements that auditors and payers scrutinize closely.
Privacy and security
The integration operates under healthcare-specific privacy standards that work with Checkpoint's existing security. Your client information never gets used for AI training.
Session recordings get deleted after the note has been reviewed. Only approved clinical documentation stay within Checkpoint, maintaining established privacy protocols.
Getting started
Look, we get it. You've probably heard promises about technology making your life easier before.
Maybe you've tried voice-to-text that couldn't tell the difference between "affect" and "effect." Or documentation software that felt like learning a new language.
This is different.
Upheal works within the Checkpoint system you already trust, with AI that actually understands the nuance of therapeutic conversations.
The clinicians already using this integration aren't just saving time. They're rediscovering why they love this work.
When documentation stops being a chore that follows you home, you get to be more present during sessions.
When you're not mentally planning how to capture complex therapeutic moments in notes, you can focus entirely on the person sitting across from you.
That's what matters most. Not the technology itself, but what it gives back to you: time with your clients, energy for your own life, and space to remember that therapeutic relationships are what drew you to this profession in the beginning.
Ready to see what Thursday evenings could look like without a documentation backlog? Join the waitlist for Checkpoint's AI integration. Your future self — and your clients — will thank you.








![5 best AI scribes for therapists [2025]](https://cdn.prod.website-files.com/6328c07d72b05347cc236c49/68a793de80a95d779e3f6814_best%20ai%20scribe%20for%20therapists%20thumbnail.avif)

